Cardionerds: A Cardiology Podcast

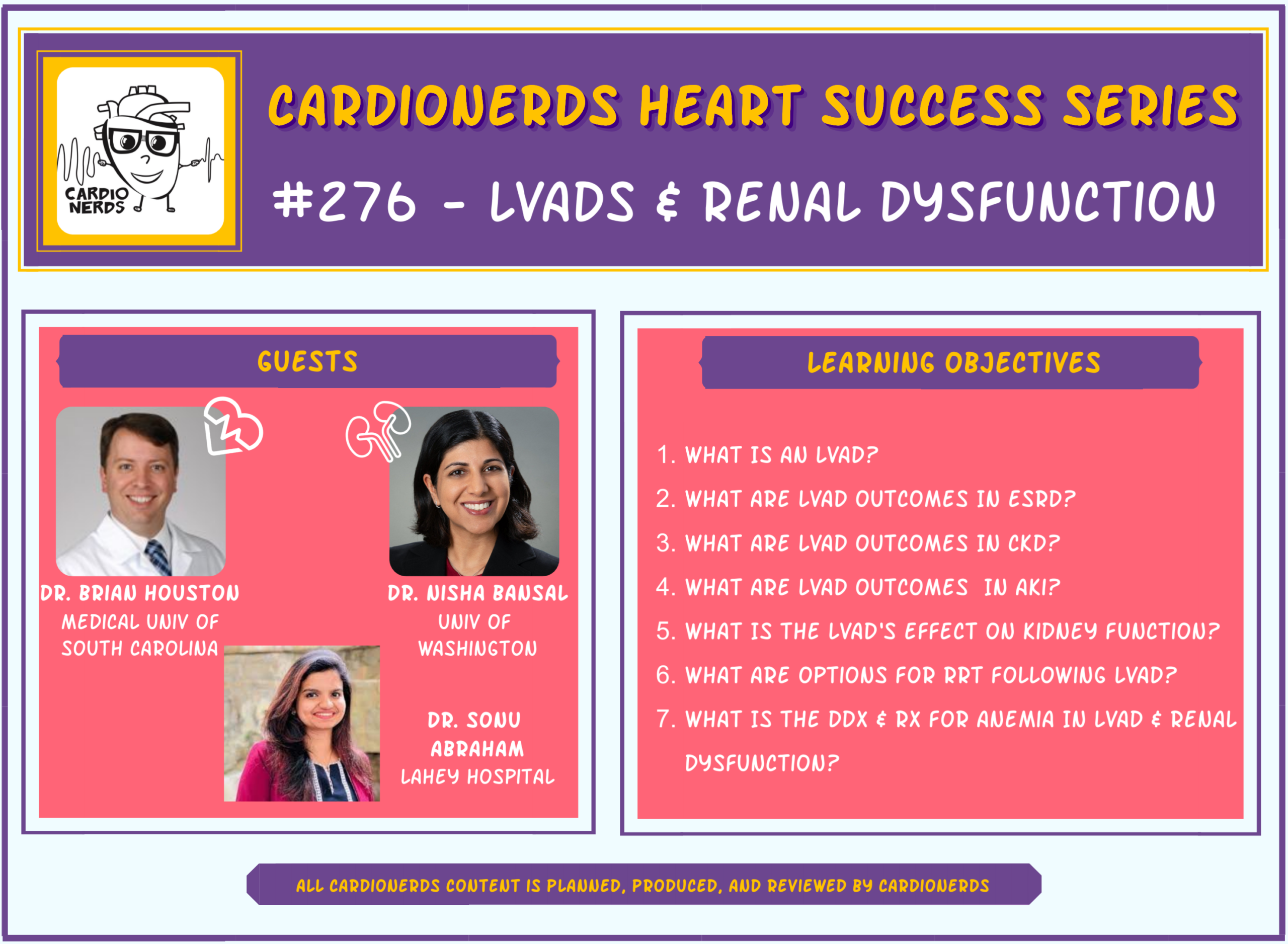
276. Left Ventricular Assist Devices and Renal Dysfunction with Dr. Brian Houston and Dr. Nisha Bansal
CardioNerds (Dr. Amit Goyal), Dr. Sonu Abraham (CardioNerds Ambassador from Lahey Hospital and Medical Center, Burlington, MA) discuss left ventricular assist devices (LVAD) and the implications of renal dysfunction with Dr. Brian Houston and Dr. Nisha Bansal. This episode will focus on the intersection of left ventricular assist devices and renal dysfunction. Patients with a combination of heart failure and renal dysfunction overall have a guarded prognosis and their management poses unique challenges to the clinician. We initially discuss the basics of an LVAD and general approach to LVAD candidacy evaluation. We then discuss specific implications of acute kidney injury, presence of preexisting CKD, and end stage renal disease in patients with/being considered for an LVAD. Risk factor identification and prognostication allows for appropriate selection of the right candidates for an LVAD in the context of renal disease. Dr. Brian Houston is the Director of the Mechanical Circulatory Support program at Medical University of South Carolina. Dr. Nisha Bansal is an Associate Professor and the Arthur Stach Family Endowed Professor in the Division of Nephrology, an investigator at the Kidney Research Institute, the Director of Nephrology Clinical and Research Education, and the Director of the Kidney-Heart Service at the University of Washington. Notes were drafted by Dr. Sonu Abraham and episode audio was edited by student Dr. Chelsea Amo-Tweneboah.
Check out the CardioNerds Failure Heart Success Series Page for more heart success episodes and content!
CardioNerds Heart Success Series Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!
Pearls – Left Ventricular Assist Devices and Renal Dysfunction
- End stage renal disease (CKD on dialysis) is considered an absolute contraindication for LVAD implantation. Select young patients who are being considered for heart-kidney transplantation in the near future may be candidates for an LVAD as a bridge to heart-kidney transplantation.
- LVAD implantation can improve kidney function in the short term in patients with AKI primarily caused by cardio-renal syndrome.
- Patients with pre-existing CKD (not dialysis dependent) have a greater risk of developing AKI after LVAD implantation.
- Several dialysis modalities including in-center hemodialysis, home hemodialysis, and peritoneal dialysis are available for LVAD patients. However, there are several challenges associated with each modality.
- An AV graft is a useful vascular access option in LVAD patients undergoing hemodialysis due to a lower risk of infection and ease of immediate use.
- Causes for anemia in patients with an LVAD and renal dysfunction include anemia of chronic disease, gastrointestinal bleeding, and pump thrombosis leading to hemolysis.
Show notes – Left Ventricular Assist Devices and Renal Dysfunction
Notes: (drafted by Dr. Sonu Abraham)
What is a left ventricular assist device (LVAD) and what are its components?
An LVAD supports circulation by unloading the left ventricle and providing increased cardiac output to help support organ perfusion. Use in properly selected patients is associated with improved quality of life and increased survival. The current iteration of LVADs offer continuous flow, as opposed to the older versions which employed pulsatile flow.
Components of the LVAD:
- Inflow cannula (sucks blood from the LV)
- Pump
- Outflow cannula (dumps blood into the aorta)
- Percutaneous driveline
- Electrical controller
How is a patient evaluated for LVAD candidacy?
The 2 main questions to be answered during the evaluation of a patient for an LVAD are:
1. Are they sick enough? Do they have end stage heart failure?
2. Do we expect the benefits of an LVAD to outweigh the risks?
- Presence/absence of right ventricular failure
- Other life limiting organ failure: Kidney failure/lung disease/liver failure/vascular disease
- Anatomic concerns (ex. LV size)
- Surgical risk (ex. Prior sternotomies, calcified aorta, etc)
- Psychosocial aspects
- Shared decision making (Does the patient want the device?)
What are the outcomes of patients with end stage renal disease (chronic kidney disease on dialysis) after LVAD implantation?
- Patients with ESRD have a high burden of comorbidities. 40% of dialysis patients have heart failure.
- The combination of heart failure and ESRD propounds a poor prognosis. Patients with ESRD without heart failure have a 40% survival in 5 years. Conversely, those with ESRD and heart failure have a < 20% survival in 5 years.
- A retrospective analysis of the United States Renal Data System revealed that 50% patients on dialysis who received an LVAD died during the index hospitalization, compared to those not on dialysis whose in hospital mortality was <10%. The median survival was ~3 weeks. By 6 months after LVAD implantation, ~70% of patients on dialysis had died.
- Based on INTERMACS data, kidney function is one of the strongest predictors of outcomes in patients with an LVAD.
What are the specific situations in which an LVAD might be offered to a patient with ESRD?
- We may consider LVAD implantation in ESRD patients under specific circumstances.
- Young patients with good functional status and good end organ function otherwise, who may be a candidate for heart-kidney transplantation in the near future, may be considered for LVAD implantation as a bridge to heart-kidney transplantation.
- If it is felt that the patient’s renal dysfunction can be improved by augmenting cardiac output and the hemodynamics suggest cardio-renal syndrome, in very select patients on recently initiated dialysis LVAD implantation may be considered. Renal imaging showing absence of scarring and the absence of proteinuria suggest a better prognostic sign and may suggest cardio-renal syndrome.
In patients with acute kidney injury (with no prior history of CKD) being evaluated for LVAD implantation, what is the effect of an LVAD on kidney function?
- Effect of an LVAD on kidney function: There is typically an initial improvement in kidney function, particularly in the first month post-implantation, due to restoration of normal hemodynamics with improvement in cardiac output and relieving renal venous congestion. Long term data, however, suggests gradual deterioration of kidney function in the long term. This is possibly due to kidney insults from the LVAD itself. The continuous flow of the LVAD can lead to periarteritis, hyperplasia of the renal arterial smooth muscle cells, and neurohormonal activation of the RAAS system leading to kidney injury over time.
- Creatinine may not be the best marker of kidney function in these patients. Cystatin C and tubular kidney injury markers, soon to be commercially available, may be better markers of kidney function.
Does having chronic kidney disease (not dialysis dependent) increase the risk of worsening kidney function after LVAD implantation?
The occurrence of AKI after LVAD worsens outcomes. The presence of CKD prior to LVAD implantation increases this risk of AKI after LVAD implantation. Patients with CKD stage 3 or more have a 1-year mortality of >30% after LVAD implantation. In patients who have AKI after LVAD implantation, 30-day mortality is 18% and 1 year mortality is 40% with increased risk of infection, multisystem organ failure, and longer length of stay.
Common causes of AKI after LVAD implantation include:
- Right ventricular failure
- Bleeding requiring blood products and crystalloids, contributing to congestion.
- Longer cardio-pulmonary bypass
Hemolysis
Based on a 10-year case series from the Mayo clinic, 15% of patients with LVAD require renal replacement therapy. If GFR<45 and there is proteinuria, the risk increased to 40%.
The 4 risk factors to predict AKI and RRT requirement after LVAD:
- Presence of a low GFR
- Proteinuria
- Increased RA pressure
- Longer cardio-pulmonary bypass time
- The HEARTMATE III Risk Score provides individual survival prediction at 1- and 2-years post LVAD implantation – includes BUN and sodium levels
What are the options available to patients in terms of long-term dialysis once LVAD patients are dialysis dependent?
- There are 3 main options for long term RRT:
- In-center hemodialysis
- Home hemodialysis
- Peritoneal dialysis
- In-center hemodialysis
- Considerations:
- In center Hemodialysis:
- Challenges: large ultrafiltration rates can lead to lower MAPs, anticoagulation considerations (bleeding complications), high risk of infection (central venous catheter), pragmatic challenges (technical expertise of the dialysis staff, comfort of the attending nephrologist, transportation issues).
- Challenges: large ultrafiltration rates can lead to lower MAPs, anticoagulation considerations (bleeding complications), high risk of infection (central venous catheter), pragmatic challenges (technical expertise of the dialysis staff, comfort of the attending nephrologist, transportation issues).
- Peritoneal dialysis:
- Benefits: decreased risk of infection (however anatomical considerations with respect to proximity to the driveline should be taken into account), more physiological and less hemodynamic instability, no need for anticoagulation.
- Challenge: home based therapy (burden on the patient and family members)
- Benefits: decreased risk of infection (however anatomical considerations with respect to proximity to the driveline should be taken into account), more physiological and less hemodynamic instability, no need for anticoagulation.
- In center Hemodialysis:
What are the options in terms of vascular access in patients with an LVAD who are started on hemodialysis?
- Central venous HD catheters – high risk of infection and therefore, not preferred.
- AV fistula – low rates of infection, however, it takes 2-3 months for fistula maturation.
- AV graft – preferred due to lower risk of infection, ability to use immediately.
What are the causes for anemia in patients with an LVAD and renal dysfunction?
- Anemia of chronic disease
- Increased risk of gastrointestinal bleed
- Anticoagulation requirement
- Acquired Von Willebrand deficiency
- Higher burden of arterio-venous malformations
- Anticoagulation requirement
- Pump thrombosis can lead to hemolysis
What are the implications of blood transfusions and use of erythropoietin stimulating agents (ESAs) in these patients?
- Judicious use of blood transfusions is advised particularly in patients waiting for a heart transplantation due to increased risk of antigen sensitization which can limit their potential donor pool.
- Those who receive ESAs have a dose-dependent increased risk of pump thrombosis and all-cause mortality. This was however, studied in patients with a HEARTMATE II (axial flow device) as opposed to the currently most commonly used pump which is the HEARTMATE III (centrifugal flow device) known to have an overall lower risk of pump thrombosis.
References
- Peritoneal Dialysis Following Left Ventricular Assist Device Placement and Kidney Recovery: A Case Report Kidney Med. 2021;3(3):438-441. Published 2021 Feb 17. doi:10.1016/j.xkme.2020.12.009
- Bansal N, Hailpern SM, Katz R, et al. Outcomes Associated With Left Ventricular Assist Devices Among Recipients With and Without End-stage Renal Disease. JAMA Intern Med. 2018;178(2):204-209. doi:10.1001/jamainternmed.2017.4831
- Butler J, Geisberg C, Howser R, et al. Relationship between renal function and left ventricular assist device use. Ann Thorac Surg. 2006;81(5):1745-1751. doi:10.1016/j.athoracsur.2005.11.061
- Haglund NA, Feurer ID, Dwyer JP, et al. Does renal dysfunction and method of bridging support influence heart transplant graft survival?. Ann Thorac Surg. 2014;98(3):835-841. doi:10.1016/j.athoracsur.2014.05.059
- Jawaid O, Gaddy A, Omar HR, Guglin M. Ventricular Assist Devices and Chronic Kidney Replacement Therapy: Technology and Outcomes. Adv Chronic Kidney Dis. 2021;28(1):37-46. doi:10.1053/j.ackd.2021.01.002
- Ootaki C, Yamashita M, Ootaki Y, et al. Reduced pulsatility induces periarteritis in kidney: role of the local renin-angiotensin system. J Thorac Cardiovasc Surg. 2008;136(1):150-158. doi:10.1016/j.jtcvs.2007.12.023
- Patel AM, Eduardo Rame J, Rudnick MR. How does the nephrologist manage an LVAD patient on chronic maintenance dialysis?. Semin Dial. 2014;27(3):284-288. doi:10.1111/sdi.12229
- Roehm B, Vest AR, Weiner DE. Left Ventricular Assist Devices, Kidney Disease, and Dialysis. Am J Kidney Dis. 2018;71(2):257-266. doi:10.1053/j.ajkd.2017.09.019
- Sandner SE, Zimpfer D, Zrunek P, et al. Renal function and outcome after continuous flow left ventricular assist device implantation. Ann Thorac Surg. 2009;87(4):1072-1078. doi:10.1016/j.athoracsur.2009.01.022
- Wettersten N, Estrella M, Brambatti M, et al. Kidney Function Following Left Ventricular Assist Device Implantation: An Observational Cohort Study. Kidney Med. 2021;3(3):378-385.e1. Published 2021 Apr 2. doi:10.1016/j.xkme.2021.01.009
- Yalcin YC, Muslem R, Veen KM, et al. Impact of Continuous Flow Left Ventricular Assist Device Therapy on Chronic Kidney Disease: A Longitudinal Multicenter Study. J Card Fail. 2020;26(4):333-341. doi:10.1016/j.cardfail.2020.01.010
- Yoshioka D, Sakaguchi T, Saito S, et al. Predictor of early mortality for severe heart failure patients with left ventricular assist device implantation: significance of INTERMACS level and renal function. Circ J. 2012;76(7):1631-1638. doi:10.1253/circj.cj-11-1452






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast