Cardionerds: A Cardiology Podcast

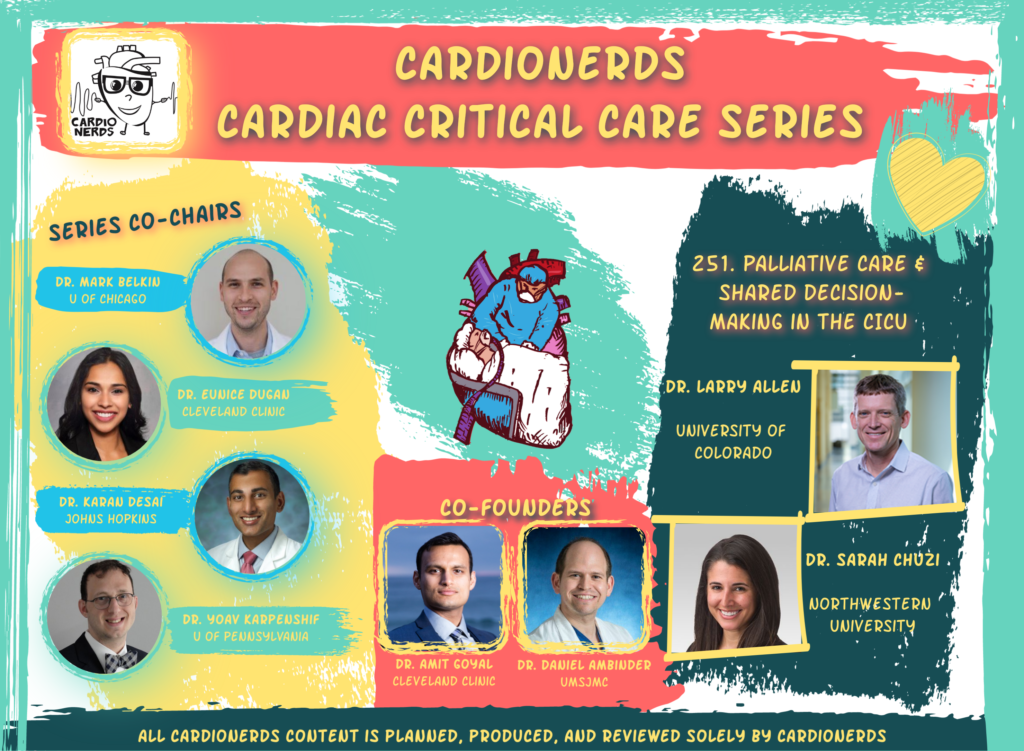
251. CCC: Palliative Care and Shared Decision-Making in the CICU with Dr. Larry Allen
This episode is focused on Palliative Care and Shared Decision-Making in the CICU. In this episode, we learn about how the principles of palliative care and shared decision-making apply to our patients across the spectrum of cardiovascular care, especially in the cardiac intensive care unit. We discuss pivotal trials of specialty palliative care and decision aids in cardiology and how they might inform our practice to enhance patient quality of life and improve goal-concordant care. Finally, we discuss practical tips and communication strategies for how to engage patients about end-of-life decisions and topics that can be utilized from outpatient to inpatient to critical care settings.
“We need to help patients hope for the best and plan for the worst as time goes on.”
Dr. Larry Allen
Series co-chairs Dr. Eunice Dugan and Dr. Karan Desai, along with CardioNerds Co-founder Amit Goyal are joined by FIT lead, Dr. Sarah Chuzi. Dr. Chuzi is a Chicagoan and completed her internal medicine residency, cardiology fellowship, AHFTC fellowship and is now Assistant Professor at Northwestern University. Our episode expert is a true national leader in shared decision-making and palliative care in heart failure – Dr. Larry Allen, Medical Director of Advanced Heart Failure and the Co-Director of the Colorado Program for Patient-Centered Decisions at the University of Colorado School of Medicine. Audio editing by CardioNerds Academy Intern, Dr. Christian Faaborg-Andersen.
The CardioNerds Cardiac Critical Care Series is a multi-institutional collaboration made possible by contributions of stellar fellow leads and expert faculty from several programs, led by series co-chairs, Dr. Mark Belkin, Dr. Eunice Dugan, Dr. Karan Desai, and Dr. Yoav Karpenshif.
Pearls • Notes • References • Production Team
CardioNerds Cardiac Critical Care Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!
Pearls and Quotes – Palliative Care and Shared Decision-Making in the CICU
1. “Much of what we do in cardiology is thinking about how to make people feel better (not just improving cardiac function or length of life). So, on a day-to-day basis we are really providing primary palliative care.” – Dr. Larry Allen
2. “Risk models in cardiology can only be so accurate… While risk models can give us some grounding, we also need to embrace the concept of uncertainty, and help patients understand that there are a variety of things that might happen to them, suggest some things they might plan for, and continue to iteratively come back to the patient and reevaluate what their options are.” – Dr. Larry Allen
3. “Our goal is to help people live happy, healthy, full lives. But, everyone dies. So understanding that death is a part of life and understanding how to help them make those transitions is critical” – Dr. Larry Allen
4. “Having good deaths is a part of good healthcare. We can’t ignore that. We can’t fight against it. We should embrace it. And we have the opportunity to do that.” – Dr. Larry Allen
5. We should still keep in mind the concept of medical futility and determining what options are reasonable for patients. Part of shared decision-making includes discussing what interventions would not be feasible or helpful with patients and families
Show notes – Palliative Care and Shared Decision-Making in the CICU
Notes drafted by Dr. Sarah Chuzi.
1. How are the basic principles of palliative care relevant to cardiology, and can you define the key concepts of shared decision-making, primary palliative care, specialty (or secondary) palliative care, and hospice care?
- Throughout medicine, we confront the concepts of symptom control, difficult medical decision-making, and end-of-life. These are the principles of palliative care and they apply very easily across the spectrum of cardiology.
- Shared decision-making is a meeting between two experts – the patient and the clinician. The patient is the expert in what’s important to them and their hopes, fears, values, goals, and preferences. The clinician is the expert in the medical aspects of care, including care that is not possible, care that might be high value, and the potential trade-offs and range of outcomes involved in a medical decision.
- Palliative care is defined by the WHO – as care that deals with patient symptoms and quality of life. Increasingly, the terms primary and secondary palliative care are used. Primary palliative care is care provided by a general clinician (or cardiologist), while secondary palliative care is provided by a board-certified palliative care clinician.
- Hospice care is really a health insurance benefit that provides a certain group of services (e.g. nurses, equipment) for patients who have terminal illness and less than 6 months to live.
2. What have we learned from existing trials looking at specialty palliative care in heart failure?
- A few large trials (CASA, ENABLE, SWAP-HF, PAL-HF) of specialty palliative care interventions in heart failure have shown mixed results.
- One of the reasons for this is the heterogeneity in patient and caregiver adjustment/symptoms at baseline.
- Future trials will need to determine which patients and caregivers are really in need of interventions or assistance surrounding some of these issues.
3. What are some strategies trainees can use to help elucidate a patient’s goals and values and engage in shared decision-making in high intensity, critical care situations?
- Trying to determine (from the patient or family) whether the patient is a medical maximizer or minimizer can be helpful; i.e., what is his preference for aggressiveness of care.
- Obtaining collateral from a patient’s power of attorney/next of kin/proxy about prior discussions regarding goals and values is valuable.
- We should still keep in mind the concept of medical futility and determining what options are reasonable for patients. Part of shared decision-making includes discussing what interventions would not feasible or helpful with patients and families.
4. What is the role of decision aids in the process of deciding whether to pursue LVAD implantation?
- Decision aids are unique from educational materials in that decision aids discuss alternative treatment options, including what life might be like if a certain treatment option is not pursued. Decision aids encourage patients to reflect on their values and then try to map the decisions in the context of their values.
- The research group at the University of Colorado developed a decision aid to help patients and their families determine whether an LVAD would be an appropriate medical intervention for them. The decision aid is available online (patientdecisionaid.org) and includes a 26-minute video and an 8-page pamphlet. Currently, they are being disseminated nationally in a large implementation trial. The DECIDE-LVAD trial demonstrated that this decision aid improved values-choice concordance for patients considering LVAD therapy.
5. What are the benefits of hospice for patients with cardiac disease and how does hospice fall short?
- It’s important to understand what hospice will and will not cover. The hospice benefit is a fixed payment per day. So, it’s important to consider what treatments might be covered and to discuss this with patients and families.
- For patients with advanced cardiac disease, coverage of inotropes is a common issue that we encounter. It’s important to prepare patients for the fact that inotropes may not be accepted in a given hospice program.
- Additionally, sometimes clinicians struggle with how to continue to provide care for patients who enter hospice as we try to navigate how to stay involved in their care while respecting their wishes to be at home and not necessarily come to clinic.
References – Palliative Care and Shared Decision-Making in the CICU






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast