Cardionerds: A Cardiology Podcast

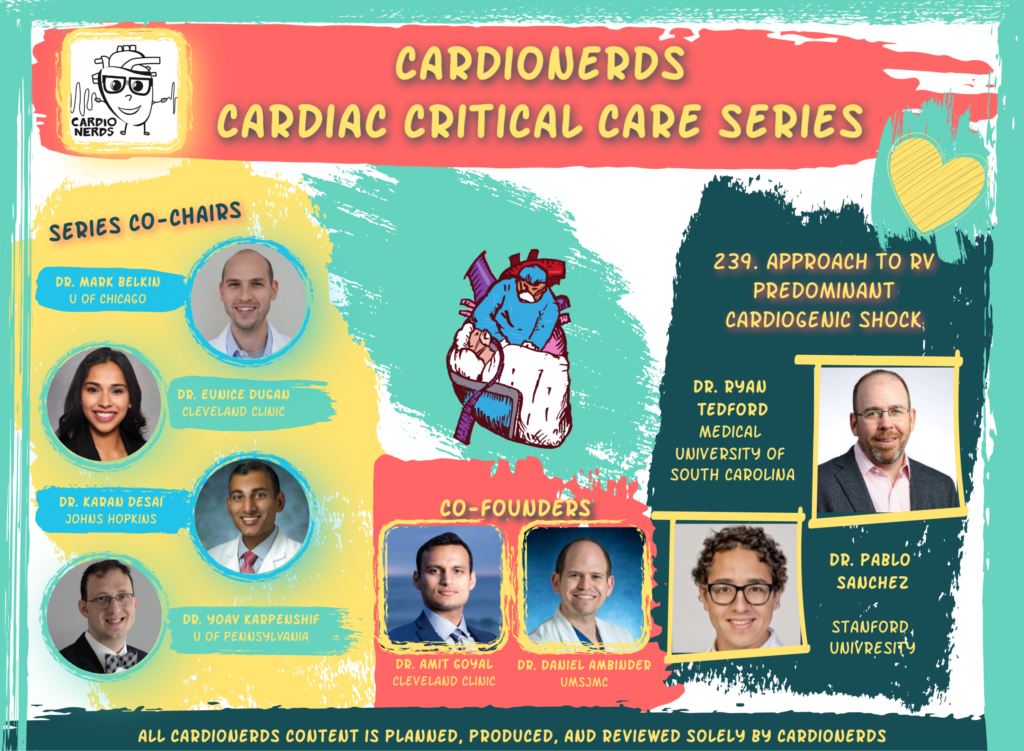
239. CCC: Approach to RV Predominant Cardiogenic Shock with Dr. Ryan Tedford
CardioNerd (Daniel Ambinder) and series co-chairs Mark Belkin (AHFT Fellow, University of Chicago) and Karan Desai (Cardiologist, Johns Hopkins), join fellow lead, Dr. Pablo Sanchez (FIT, Stanford) for a discussion with Dr. Ryan Tedford (Professor of Medicine at the Medical University of South Carolina) about Right Ventricular (RV) predominant cardiogenic shock. In this episode we explore risk factors, pathophysiology, hemodynamics, and treatment strategies in this common and complex problem. We dissect three cases that epitomize the range of diagnostic dilemmas and management decisions in RV predominant shock, as Dr. Tedford expertly weaves us through the pathophysiology and decision-making involved in managing the “people’s ventricle.” Audio editing by Dr. Gurleen Kaur (Director of the CardioNerds internship program, CardioNerds academy fellow, and IM resident at Brigham and Women’s Hospital).
The CardioNerds Cardiac Critical Care Series is a multi-institutional collaboration made possible by contributions of stellar fellow leads and expert faculty from several programs, led by series co-chairs, Dr. Mark Belkin, Dr. Eunice Dugan, Dr. Karan Desai, and Dr. Yoav Karpenshif.
Pearls • Notes • References • Production Team
CardioNerds Cardiac Critical Care Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!
Pearls and Quotes – RV Predominant Cardiogenic Shock
- The degree of RV dysfunction and failure are modulated by stretching its capacity to tolerate insults from deranged afterload, preload, and contractility.
- Afterload insults are MUCH LESS tolerated than other insults and broadly comprise the most common pathophysiologic cause of both acute and chronic RV failure.
- RV and left ventricular (LV) function are anatomically and physiologically connected. Progressive derangements in RV function can lead to the deadly “RV spiral,” in which poor RV function causes lower LV preload, leading to hypotension, and thus worsening RV perfusion and function.
- In RV failure/shock, some basic tenets including treating reversible causes, optimizing preload and afterload, and using inotropes and/or temporary MCS for as limited time as possible.
- Many acute RV failure patients can recover, but multiorgan injury plays an important role. Therefore, thoughtful and expeditious use of mechanical circulatory support is important.
Show notes – RV Predominant Cardiogenic Shock
Notes drafted by Dr. Pablo Sanchez.
- What is the basic difference between RV dysfunction and failure?
- Dysfunction: Abnormalities in systolic/diastolic function of the RV, but not necessarily to the point of leading to end-organ perfusion defects. RV dysfunction leads to poor outcomes regardless of mechanism.1
- Failure: Clinical syndrome of inability of RV to maintain adequate output despite adequate preload. 1
- Dysfunction: Abnormalities in systolic/diastolic function of the RV, but not necessarily to the point of leading to end-organ perfusion defects. RV dysfunction leads to poor outcomes regardless of mechanism.1
- How is the RV different from the LV and what impact does it have on pathophysiology and hemodynamics?
- The LV and RV originate from different embryologic “heart fields.”1,2
- The RV wall is thinner and more compliant and has only two layers (instead of 3 like the LV).3 Furthermore, unlike the LV which has a significant proportion of endocardial and epicardial transverse myocardial fibers, the RV myocardial fibers are aligned in a longitudinal plane for the most part. Thus, a more significant proportion of RV systolic contraction is longitudinal – base of the ventricle moving towards the apex.
- The RV is crescent-shaped and has a large surface-to-volume ratio meaning smaller inward motion ejects the same stroke volume. 1
- Hemodynamically, the RV takes blood from a low-pressure venous system and gives it to a distensible system with low impedance (the normal pulmonary circuit at baseline typically has a resistance one-tenth of the systemic resistance). Therefore, volume loads (preload) are much better handled than pressure (afterload).1
- The LV and RV originate from different embryologic “heart fields.”1,2
- What is RV-PA coupling?
- As Dr. Tedford noted, RV-PA coupling describes “the interaction of RV contractility and afterload (resistive and pulsatile components). It is the most comprehensive description of RV function and therefore the Gold Standard.” Whether we are referring to the LV or RV, the basic concept of coupling describes the energy transfer between ventricular contractility and arterial afterload.
- RV-PA coupling has typically been assessed by pressure-volume loops, with ventricular contractility assessed by end-systolic elastance (a load-independent measure of systolic function) and arterial afterload by effective arterial elastance.
- MODUS OPERANDI: RV dysfunction and eventual failure is modulated by stretching its capacity to tolerate insults from afterload, preload, and contractility.
- As Dr. Tedford noted, RV-PA coupling describes “the interaction of RV contractility and afterload (resistive and pulsatile components). It is the most comprehensive description of RV function and therefore the Gold Standard.” Whether we are referring to the LV or RV, the basic concept of coupling describes the energy transfer between ventricular contractility and arterial afterload.
- What leads to ACUTE right heart failure?
- Most commonly results from:1
- Abrupt increases in afterload (e.g., think PE, hypoxia, and acidemia).
- Decreased contractility (e.g., think ischemia such as RV infarction, myocarditis, and post-cardiotomy).
- Volume overload can sometimes lead to acute right heart failure, particularly in the setting of another categorical insult such as septic cardiomyopathy or LVAD support.
- Most commonly results from:1
- What leads to CHRONIC right heart failure?
- This is different than acute right heart failure. Most commonly chronic right heart failure results from:1
- Gradual increases in afterload (e.g., think pulmonary arterial hypertension).
- Chronic volume overload (e.g., longstanding tricuspid regurgitation, atrial septal defect, and other congenital lesions like double outlet RV).
- Contractility (e.g., including the isolated RV cardiomyopathies like arrhythmogenic right ventricular cardiomyopathy or ischemic cardiomyopathy).
- Other pathologies certainly affect multiple categories (e.g., Ebstein’s anomaly which is a function of contractility and volume overload or single ventricle physiology like post-Fontan patients – for more on these and other ACHD lesions, enjoy the CardioNerds ACHD Series!)
- Gradual increases in afterload (e.g., think pulmonary arterial hypertension).
- MODUS OPERANDI: The cardiovascular system is wholly connected, and acute decompensation leads to progressive derangements in the above levers (including LV function). This phenomenon is called the RV spiral.
- This is different than acute right heart failure. Most commonly chronic right heart failure results from:1
- How do we manage RV failure?
- The most important and first step is the treatment of reversible causes. For instance, acute coronary syndrome involving the RV requires percutaneous intervention (PCI) or pulmonary embolism requires anticoagulation and/or thrombolytic/device/surgical therapy.
- PRELOAD OPTIMIZATION
- Ensuring that there is adequate preload is a key tenet of diagnosing and treating RV failure. This may require diuresis or judicious volume resuscitation to maintain cardiac output.
- While guiding fluid management in the setting of RV failure, one should STRONGLY consider invasive hemodynamic monitoring (e.g., over-resuscitation can lead to decreased LV output through septal shift and ventricular interdependence from pericardial constraint).1
- General target: We could consider a CVP 10-15 mmHg; however, this will be individualized. Another general rule would also be if that a bolus of 500 cc of crystalloid does not result in hemodynamic improvement, further loading should not be continued, especially without invasive hemodynamic guidance.
- Ensuring that there is adequate preload is a key tenet of diagnosing and treating RV failure. This may require diuresis or judicious volume resuscitation to maintain cardiac output.
- AFTERLOAD OPTIMIZATION
- The goal should be to correct reversible causes of elevated pulmonary vascular resistance (e.g., acidosis, hypercapnia, hypoxia, and generally in ventilated patients avoid elevated inspiratory pressures > 30mmHg).1
- With specialized expert guidance, we can consider selective pulmonary vasodilators (acutely and short-term):
- One example includes inhaled NO, and in observational studies, short-term use lowered PVR and increased RV ejection.4
- We also have to remember the consequences of reducing RV afterload. Acutely increasing LV preload in a baseline abnormal LV may lead to distention, lowered cardiac output, and pulmonary edema.1
- Pulmonary vasodilators can act on specific pathways (e.g., nitric oxide, prostacyclin, endothelin-1, and soluble guanylate cyclase stimulators) and come in various forms (oral, inhaled, and intravenous).
- One example includes inhaled NO, and in observational studies, short-term use lowered PVR and increased RV ejection.4
- The goal should be to correct reversible causes of elevated pulmonary vascular resistance (e.g., acidosis, hypercapnia, hypoxia, and generally in ventilated patients avoid elevated inspiratory pressures > 30mmHg).1
- CONTRACTILITY AUGMENTATION (INOTROPES)
- We typically utilize inotropes in concert with the prior two but optimize loading so the time we need inotropes is minimal.1
- Short-term use can improve hemodynamics. Longer-term use will typically increase myocardial O2 consumption and is associated with increased mortality.
- The RV has coronary perfusion in systole and diastole, so peripheral vasopressors are helpful to maintain perfusion, especially if systolic blood pressure is less than RV systolic pressure.1
- We typically utilize inotropes in concert with the prior two but optimize loading so the time we need inotropes is minimal.1
- GOAL: Increase contractility without increasing RV afterload.
- The most important and first step is the treatment of reversible causes. For instance, acute coronary syndrome involving the RV requires percutaneous intervention (PCI) or pulmonary embolism requires anticoagulation and/or thrombolytic/device/surgical therapy.
- For those failing to respond to these above measures to optimize preload, afterload, and contractility, there may be a role for temporary mechanical circulatory support (see #10 below).
- How do we decide between dobutamine and milrinone?
- BOTH inotropes can lead to hypotension, have similar clinical outcomes, hemodynamic efficacy and arrhythmogenic potential1 (despite the adage that attributes more arrhythmias to dobutamine, studies show the risk is typically the same in both5).
- Milrinone is a more potent vasodilator (systemic and pulmonary) typically leading to greater decreases in end-diastolic pressures in the ventricles.1 It is renally cleared, has a longer half-life, and acts through a separate mechanism pathway compared to beta-blockade, thus patients can be on milrinone and beta blockers at the same time on a case-by-case basis.1
- Dobutamine has a shorter half-life, with rapid onset/offset and so may be more ideal in unstable/hypotensive patients.1
- BOTH inotropes can lead to hypotension, have similar clinical outcomes, hemodynamic efficacy and arrhythmogenic potential1 (despite the adage that attributes more arrhythmias to dobutamine, studies show the risk is typically the same in both5).
- What if the patient is hypotensive?
- In this circumstance, we would need an ino-constrictor or peripheral vasoconstrictor.
- Vasopressin has almost no impact on PVR, so unlike catecholamines, it does not directly worsen RV afterload.1
- In this circumstance, we would need an ino-constrictor or peripheral vasoconstrictor.
- What are some important invasive hemodynamic parameters to be aware of?
- RAP/PCWP ratio: Disproportionate RV dysfunction can be portrayed by an RAP/PCWP ratio > 0.5-0.8 (depending on the clinical situation). In other words, the closer that RAP and PCWP are, the more likely you have disproportionate RV dysfunction.
- The predictive power of this ratio is different depending on the situation. Pre-operatively, a ratio > 0.63 is associated with RHF post-LVAD.6 In acute inferior MI, a ratio of > 0.86 is associated with RHF.7
- The predictive power of this ratio is different depending on the situation. Pre-operatively, a ratio > 0.63 is associated with RHF post-LVAD.6 In acute inferior MI, a ratio of > 0.86 is associated with RHF.7
- PAPi: The PA pulse pressure gives us an idea of the ability of the RV to generate SV. Dividing this by the RAP, gives us an index that takes into account right-sided filling pressures.
- As above, the context is important. In acute inferior MI a PAPi of < 1.0 is predictive of mortality or MCS need,8 while a pre-operative PAPi < 1.8 was predictive of RHF after LVAD.9
- Caveats: As Dr. Tedford mentioned, the PAPi is related to RV function, but not a direct measure of it. Manipulation of each component (e.g., pulse pressure or RA pressure) can ultimately lead to a similar absolute value of PAPi under very different loading conditions.
- PA pulse pressure is a function not only of SV but also of PA capacitance. In other words, a narrow pulse pressure can be due to a failing RV or a low pulmonary capacitance (from fluid overload for example). This isn’t clearly gleaned from the PAPi alone and requires us to keep in mind the context of the equation.
- As above, the context is important. In acute inferior MI a PAPi of < 1.0 is predictive of mortality or MCS need,8 while a pre-operative PAPi < 1.8 was predictive of RHF after LVAD.9
- Note: The gold standard assessments of RV contractility are derived from Pressure-Volume loops which require both simultaneous assessment of pressure and volume as well as alteration of preload over multiple beats. This limits applicability because it is technically challenging to do.10
- RAP/PCWP ratio: Disproportionate RV dysfunction can be portrayed by an RAP/PCWP ratio > 0.5-0.8 (depending on the clinical situation). In other words, the closer that RAP and PCWP are, the more likely you have disproportionate RV dysfunction.
- What are important concepts to remember for Mechanical Support of the RV?
- One of the first things to consider is the end-game: are we using MCS as a bridge to recovery, bridge to decision, bridge to transplant, or bridge to durable MCS?
- Many acute RHF patients can recover with adequate support and a significant prognostic factor is preventing multiorgan failure.11,12 If MCS is needed, early use is better than later.
- Another important question is if we need oxygenation? Many of the MCS options, except the Impella RP, can have an oxygenator spliced into the system.11
- A key question will be if we need RV-only support or biventricular support?11
- RV-targeted support will increase LV preload, and the LV has to be able to accommodate the increased volume.
- If the LV is unable to tolerate the increased return, systemic cardiac output can become inadequate, LV filling pressures will rise, which can lead to pulmonary edema and increase mean PA pressures further (which can also lead to acute lung injury and worse outcomes). In these circumstances, biventricular support with either VA-ECMO or permutations of isolated RV + LV support may be needed.
- RV-targeted support will increase LV preload, and the LV has to be able to accommodate the increased volume.
- We also have to ask ourselves, if pulmonary arterial HTN primarily responsible for RV shock?11
- If so, then VA-ECMO may be the most appropriate option.
- Increased flow from an RVAD, combined with a pre-existing elevated PVR can lead to elevated pulmonary artery pressures, which can precipitate pulmonary hemorrhage.1
- If so, then VA-ECMO may be the most appropriate option.
- One of the first things to consider is the end-game: are we using MCS as a bridge to recovery, bridge to decision, bridge to transplant, or bridge to durable MCS?
References – RV Predominant Cardiogenic Shock
CardioNerds Cardiac Critical Care Production Team
 Karan Desai, MD
Karan Desai, MD Dr. Mark Belkin
Dr. Mark Belkin Dr. Yoav Karpenshif
Dr. Yoav Karpenshif Amit Goyal, MD
Amit Goyal, MD Daniel Ambinder, MD
Daniel Ambinder, MD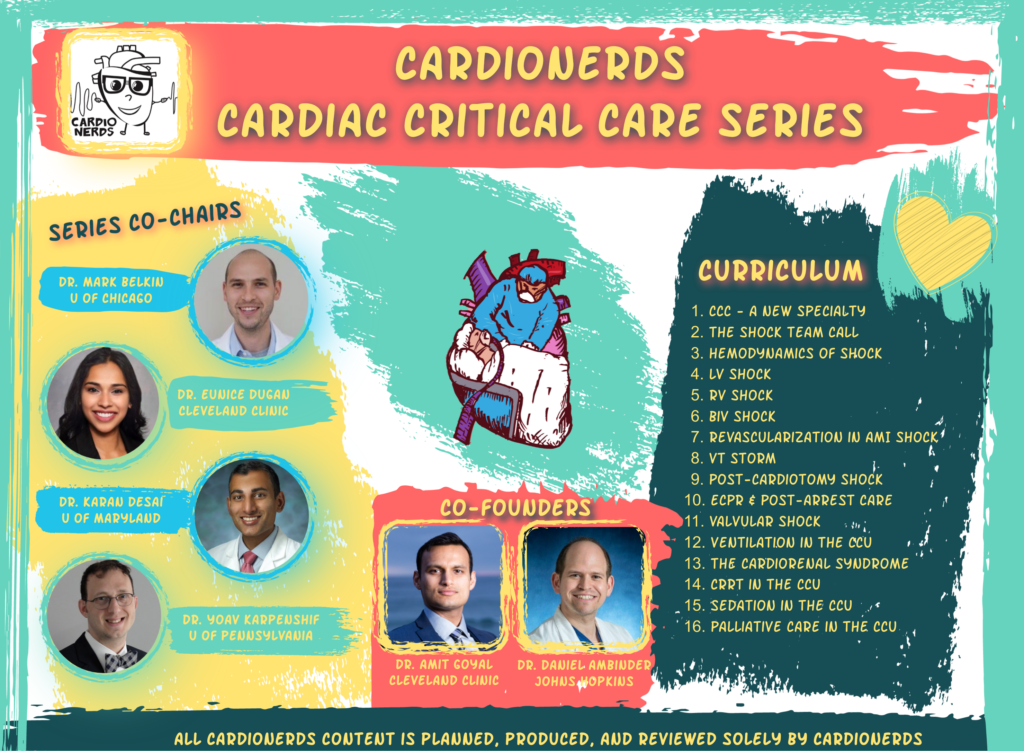






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast