Cardionerds: A Cardiology Podcast

213. ACHD: Transitions of Care in Congenital Heart Disease with Dr. Peter Ermis and Dr. Scott Cohen
CardioNerd (Amit Goyal), ACHD series co-chair Dr. Agnes Koczo (UPMC), and episode FIT lead, Dr. Logan Eberly (Emory University, incoming ACHD fellow at Boston Adult Congenital Heart) join Dr. Peter Ermis (Program Director of the Adult Congenital Heart Disease Program at Texas Children’s Heart Center), and Dr. Scott Cohen (Associate Professor and Director of the Adult Congenital Heart Disease Program at the Medical College of Wisconsin) for a discussion about transitions of care in congenital heart disease. Audio editing by Dr. Gurleen Kaur (Director of the CardioNerds Internship and CardioNerds Academy Fellow).
Congenital heart disease (CHD) is the most common clinically significant congenital defect, occurring in approximately 1 in 100 live births. With modern advances in pediatric cardiology and cardiac surgery, over 90% of children born in the developed world with CHD will now survive into adulthood, and there are currently more adults than children living with CHD in the United States1.
As these children become adults, they will need to transition their care from pediatric to adult-centered care. Unfortunately, during this transition period, there is often delayed or inappropriate care, improper timing of the transfer of care, and undue emotional and financial stress on the patients, their families, and the healthcare system. At its worst, patients are lost to appropriate follow-up. In this episode, we review the current climate in transitions of care for CHD patients from child-centered to adult-centered care, discuss the difficulties that can occur during the transitions process. We further discuss how to mitigate them, and highlight the key elements to the successful transitions of care.
The CardioNerds Adult Congenital Heart Disease (ACHD) series provides a comprehensive curriculum to dive deep into the labyrinthine world of congenital heart disease with the aim of empowering every CardioNerd to help improve the lives of people living with congenital heart disease. This series is multi-institutional collaborative project made possible by contributions of stellar fellow leads and expert faculty from several programs, led by series co-chairs, Dr. Josh Saef, Dr. Agnes Koczo, and Dr. Dan Clark.
The CardioNerds Adult Congenital Heart Disease Series is developed in collaboration with the Adult Congenital Heart Association, The CHiP Network, and Heart University. See more
Disclosures: None
Pearls • Notes • References • Guest Profiles • Production Team

CardioNerds Adult Congenital Heart Disease Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!
Pearls – Transitions of Care in Congenital Heart Disease
- There is a clear distinction between the TRANSFER of care and TRANSITION of care. Transfer is merely moving from a pediatric to adult provider. Transition involves the continuing education of the patient with regards to their congenital heart disease, the importance of longitudinal follow up, and leading patients toward more autonomous medical care. Transition begins in the pediatric cardiology clinic prior to the transfer of care and is an ongoing process that continues well after the physical transfer of care.
- A critical aspect of the transition and transfer of care is cultivating trust—that is, the new adult congenital heart disease (ACHD) provider must earn the trust of the patient and family. A failure to do so will inevitably prevent an optimal transition of care.
- During transition, parents are transitioning along with their children. With transition to adult care, there is also a goal to transition responsibility for medical care from the parent to the child. Setting goals and expectations can help both the parents and the child effectively make this transition.
- Loss to follow up is one of the most concerning complications of poor transition. Interestingly, there does not appear to be a strong association between complexity of congenital heart disease and the likelihood of loss to follow up. ACHD providers should not assume that patients with complex ACHD are less likely to be lost to follow up. For example, approximately 25-30% of Fontan patients have lapses or gaps in care. Effective transition of care is essential for all severity levels of ACHD. It is recommended in the 2018 AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease2, as well as in the 2011 AHA Scientific Statement on Best Practices in Managing Transition to Adulthood for Adolescents With Congenital Heart Disease3.
Show notes – Transitions of Care in Congenital Heart Disease
1. What is the current climate in transitions of care for patients from child-centered to adult-centered care, and what are some of the difficulties on the side of the provider as well as the patient during this process?
- Transition is a complex process, and there is no “one size fits all” approach to the effective transition of ACHD patients.
- Many patients live far away from an ACHD centers of excellence.
- There are also currently not enough ACHD cardiologists to care for ACHD patients.
- Due to these challenges, there can be anxiety with regards to transferring care to an ACHD provider from the perspective of both the patient and the pediatric cardiologist.
- This time in a young person’s life is not just a time of transition of medical care; there are many simultaneous immense life transitions as well. There may be a loss of focus on the importance of ongoing follow up in medical care.
2. What topics should be addressed at the first ACHD visit?
- The ACHD program and its relationship to both the pediatric and adult hospital should be thoroughly explained, and the patient needs to be informed where both inpatient and outpatient care take place.
- ACHD providers should ask open-ended questions to determine the patient’s understanding of their congenital heart disease and then provide education as needed.
- The first ACHD visit should focus on laying out a detailed, long-term plan of care for the patient. Patients should be advised what specifically will be monitored going forward (such as valve function, cardiac chamber size, arrhythmias, etc.), as well as what future diagnostic testing (echo, MRI/CT, stress testing, etc.) is to be expected. For female patients, contraception and the safety of pregnancy should be addressed starting in the first visit.
- One of the primary goals of the first ACHD visit is also to build trust. To this end, an ACHD provider should try to avoid any major changes to medical therapy at the first visit unless deemed absolutely necessary.
3. What are advantages and disadvantages of different models of transitions of care?
- There is no “one size fits all” model to transition, but there certainly are some guiding principles.
- Formal transition programs are important. They can help normalize transition and eliminate the sentiment that the patient is being “kicked out” of pediatric cardiology clinic. Additionally, formal transitions programs can reduce unexpected cardiac hospitalizations for ACHD patients2. This decreases the unnecessary utilization of hospital resources.
- An ACHD program that remains within a children’s hospital has the benefit that the patients are already familiar with the site, and they may also be less likely to be lost to follow up. However, there is the drawback that non-cardiology providers in a children’s hospital are often unfamiliar with the management of adult medical problems, which necessitates forming relationships with adult providers at partner institutions, and this can be challenging.
- Ultimately, ACHD patients can be cared for effectively at either a children’s hospital-based or adult hospital-based program. The model that is most effective for a particular institution is dependent upon the resources available and the investment of a supportive multi-disciplinary team.
4. What is the role of the parents in the transition process?
- Parents play a vital role in the transition process. They are often quite informed of their child’s history, so the new ACHD provider needs to carefully review the patient’s history prior to the first visit. Having thorough knowledge of a patient’s medical history will help build trust with patients and their families.
- ACHD providers should involve the parents in the transition process and should set goals and expectations. They should ask the parents to empower their child with regards to their medical care (such as encouraging them to manage their own medications, schedule their own medical appointments, etc.)
- ACHD providers need to have patience when working with parents during the transition process. Providers need to acknowledge that the parents have been the primary manager of their child’s medical care for many years, and it is often difficult to give up this role and to allow their child to be autonomous.
- It’s important to remember that parents are also transitioning. They transition from being the primary manager of their child’s health to being co-managers, before ultimately relinquishing the responsibility to their child.
5. What are some negative sequelae of a poor transition of care?
- The worst possible outcome is loss to follow up. This can result in potentially preventable medical complications.
- Inadequate or poor transition can lead to parental and/or patient distrust of the ACHD provider, which in turn increases the risk of being lost to follow up.
- Suboptimal transition increases the risk that the patient will engage in high-risk behaviors that can be harmful to their health.
- Patients who are not transitioned properly tend to utilize more hospital resources.
6. How should female ACHD patients be counseled on women’s health issues?
- In general, cardiologists are not well trained in addressing issues such as sexual health and contraception.
- However, discussions of topics such as family planning and the safety of pregnancy is important to begin during pediatric care. The longer the providers wait to address these issues, the higher the risk of unplanned pregnancy in a high-risk patient.
- Discussion of topics such as sex and contraception needs to be a routine part of every ACHD patient visit. A significant way to overcome the discomfort that both providers and patients have when talking about these issues is to make the discussion routine and therefore normal.
- There are several risk stratifications tools available (CARPREG II, modified WHO, see tables below) to help ACHD providers assess the cardiovascular risk of pregnancy for ACHD patients.
- Fortunately, overall mortality during pregnancy for ACHD patients is low, and most adult women with congenital heart disease can complete a pregnancy safely. However, close monitoring (particularly for heart failure and arrhythmias) is important.
7. What are the key elements in the successful transition of care?
- The transition process should be formal in its organization and deliberate.
- Communication is crucial, both between pediatric and adult providers, as well as between providers, patients, and their families.
- The transition and transfer of care needs to be specifically to an ACHD provider. Many ACHD patients end up under the care of general adult cardiologists, who often do not have the experience or expertise to effectively manage them. There is robust evidence that ACHD patients who do not follow at an ACHD Center of Excellence have worse outcomes. As mentioned prior, location in proximity to a Center of Excellence can be a barrier for patients when trying to complete a successful transition.
References – Transitions of Care in Congenital Heart Disease
Meet Our Collaborators!
Adult Congenital Heart Association
Founded in 1998, the Adult Congenital Heart Association is an organization begun by and dedicated to supporting individuals and families living with congenital heart disease and advancing the care and treatment available to our community. Our mission is to empower the congenital heart disease community by advancing access to resources and specialized care that improve patient-centered outcomes. Visit their website (https://www.achaheart.org/) for information on their patient advocacy efforts, educational material, and membership for patients and providers
CHiP Network
The CHiP network is a non-profit organization aiming to connect congenital heart professionals around the world. Visit their website (thechipnetwork.org) and become a member to access free high-quality educational material, upcoming news and events, and the fantastic monthly Journal Watch, keeping you up to date with congenital scientific releases. Visit their website (https://thechipnetwork.org/) for more information.

Heart University
Heart University aims to be “the go-to online resource” for e-learning in CHD and paediatric-acquired heart disease. It is a carefully curated open access library of educational material for all providers of care to children and adults with CHD or children with acquired heart disease, whether a trainee or a practicing provider. The site provides free content to a global audience in two broad domains: 1. A comprehensive curriculum of training modules and associated testing for trainees. 2. A curated library of conference and grand rounds recordings for continuing medical education. Learn more at www.heartuniversity.org/

Guest Profiles – Transitions of Care in Congenital Heart Disease
 Dr. Peter Ermis
Dr. Peter ErmisDr. Peter Ermis is the Medical Director for the Adult Congenital Heart Program at Texas Children’s Hospital and Assistant Professor at Baylor College of Medicine in Houston, TX. He earned his medical degree at the University of Texas Health Science Center in San Antonio in 2005 and later completed a combined Medicine/Pediatrics residency at Baylor College of Medicine in 2009. He then completed a combined Adult Cardiovascular Disease and Pediatric Cardiology Fellowship at Texas Children’s Hospital and the Texas Heart Institute in 2014. In addition to his role as medical director, Dr. Ermis is also the Program Director for the Adult Congenital Heart Disease Fellowship and the Head of Adult Medicine at Texas Children’s Hospital. Dr. Ermis’ interests include optimizing care for adult survivors of chronic childhood diseases, including adult congenital heart disease patients. He has been instrumental in the creation and opening of an outpatient and inpatient unit designed completely for ACHD patients at Texas Children’s Hospital which opened in 2020.
 Dr. Scott Cohen
Dr. Scott CohenDr. Scott Cohen is an Associate Professor and Director of the Adult Congenital Heart Disease Program at the Medical College of Wisconsin. He completed residency in med/peds as well as adult cardiology fellowship at the Warren Alpert Medical School of Brown University. He also completed a fellowship in both preventative medicine and ACHD at the VA in Rhode Island and then the Children’s Hospital of Wisconsin, respectively.
 Dr. Logan Eberly
Dr. Logan EberlyDr. Logan Eberly was born in New Orleans but raised in Louisville, Kentucky. He attended Duke for his combined med/peds residency, and is now a general cardiology fellow at Emory and will be joining the BACH or Boston Adult Congenital Heart (BACH) and Pulmonary Hypertension Program to continue his training. He is passionate about cardiovascular imaging, cardio-obstetrics pulmonary hypertension, medical education and global health.
CardioNerds Adult Congenital Heart Disease Production Team


 Amit Goyal, MD
Amit Goyal, MD Daniel Ambinder, MD
Daniel Ambinder, MD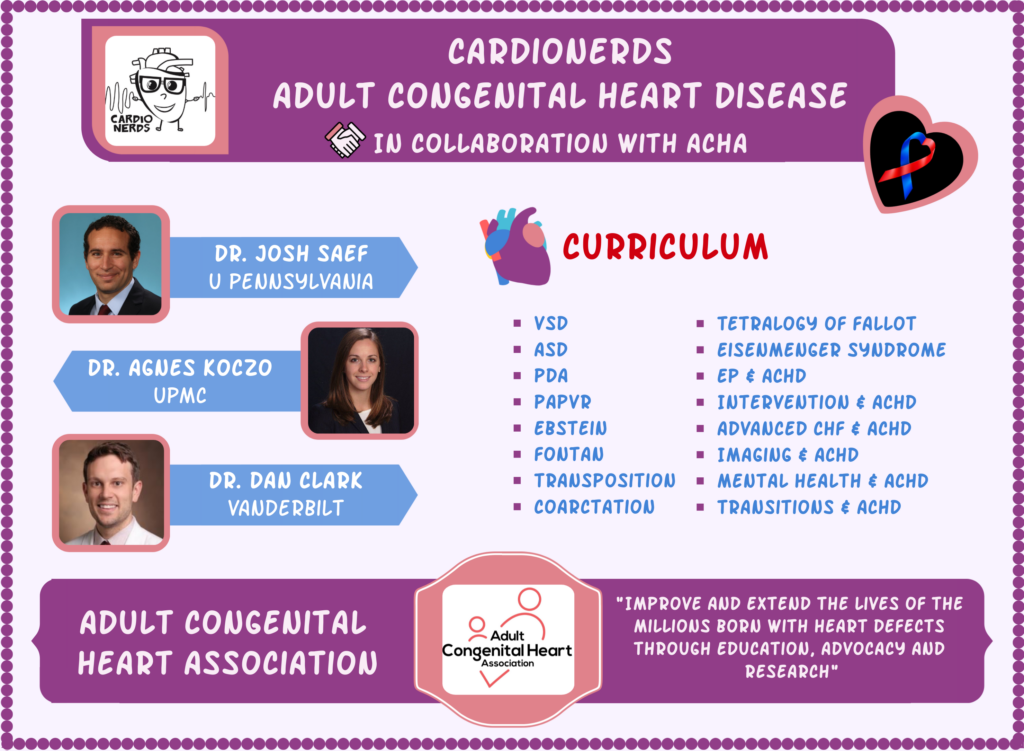






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast