Cardionerds: A Cardiology Podcast

209. CardioNerds Rounds: Challenging Cases – Modern Guideline Directed Therapy in Heart Failure with Dr. Randall Starling
It’s another session of CardioNerds Rounds! In these rounds, Co-Chairs, Dr. Karan Desai and Dr. Natalie Stokes and Dr. Tiffany Dong (FIT at Cleveland Clinic) joins Dr. Randall Starling (Professor of Medicine and Director of Heart Transplant and Mechanical Circulatory Support at Cleveland Clinic) to discuss the nuances of guideline directed medical therapy (GDMT) through real cases. As a past president of the Heart Failure Society of America (HFSA) and author on several guidelines, Dr. Starling gives us man pearls on GDMT. Come round with us today by listening to the episodes and joining future sessions of #CardsRounds!
This episode is supported with unrestricted funding from Zoll LifeVest. A special thank you to Mitzy Applegate and Ivan Chevere for their production skills that help make CardioNerds Rounds such an amazing success. All CardioNerds content is planned, produced, and reviewed solely by CardioNerds. Case details are altered to protect patient health information. CardioNerds Rounds is co-chaired by Dr. Karan Desai and Dr. Natalie Stokes.
Speaker disclosures: None
Cases discussed and Show Notes • References • Production Team
CardioNerds Rounds Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!
Show notes – CardioNerds Rounds: Challenging Cases – Modern Guideline Directed Therapy in Heart Failure with Dr. Randall Starling
Case #1 Synopsis:
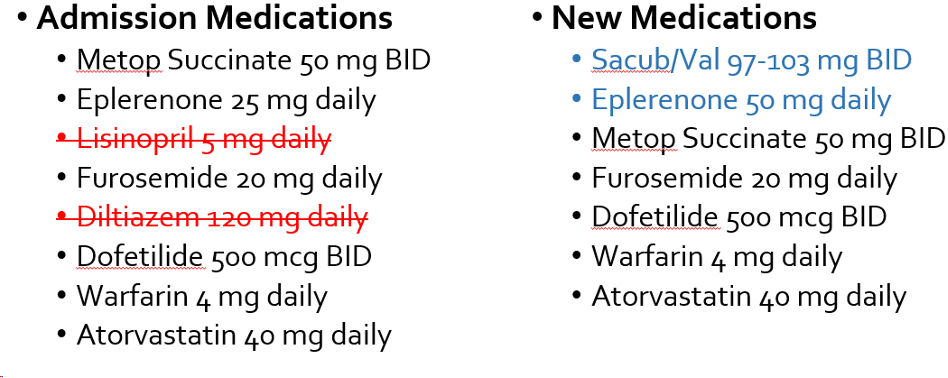
A man in his 60s with known genetic MYPBC3 cardiomyopathy and heart failure with a reduced ejection fraction of 30% presents with worsening dyspnea on exertion over the past 6 months. His past medical history also included atrial fibrillation with prior ablation and sick sinus syndrome with pacemaker implantation. Medications are listed below. He underwent an elective right heart catheterization prior to defibrillator upgrade for primary prevention. At the time of right heart catheterization, his blood pressure was 153/99 with a heart rate of 60. His RHC demonstrated a RA pressure of 15mmHg, RV 52/16, PA 59/32 (mean 41), and PCWP 28 with Fick CO/CI of 2.8 L/min and index of 1.2 L/min/m2. His SVR was 1900 dynes/s/cm-5. He was admitted to the cardiac ICU and started on nitroprusside that was transitioned to a regimen of Sacubitril-Valsartan and Eplerenone. His final RHC numbers were RA 7, PA 46/18/29, PCWP 16 and Fick CO/CI 6.1/2.6. His discharge medications are shown below.
Takeaways from Case #1
- Unless there are contraindications (cardiogenic shock or AV block), continue a patient’s home beta blocker to maintain the neurohormonal blockade benefits. A low cardiac index should be interpreted in the full context of the patient, including their symptoms, other markers of perfusion (e.g., urine output, mentation, serum lactate), and mean arterial pressure before holding or stopping beta blockade. Carvedilol, metoprolol succinate and bisoprolol are all evidence-based options for beta blockers in heart failure with reduced ejection fraction.
- If there is concern of lowering blood pressure too much with Sacubitril/Valsartan, one method is to trial low dose of valsartan first and then transition to Sac/Val. Note, in the PARADIGM-HF trial, the initial exclusion criteria for starting Sac/Val included no symptomatic hypotension and SBP ≥ 100. At subsequent up-titration visits, the blood pressure criteria was decreased to SBP ≥ 95.
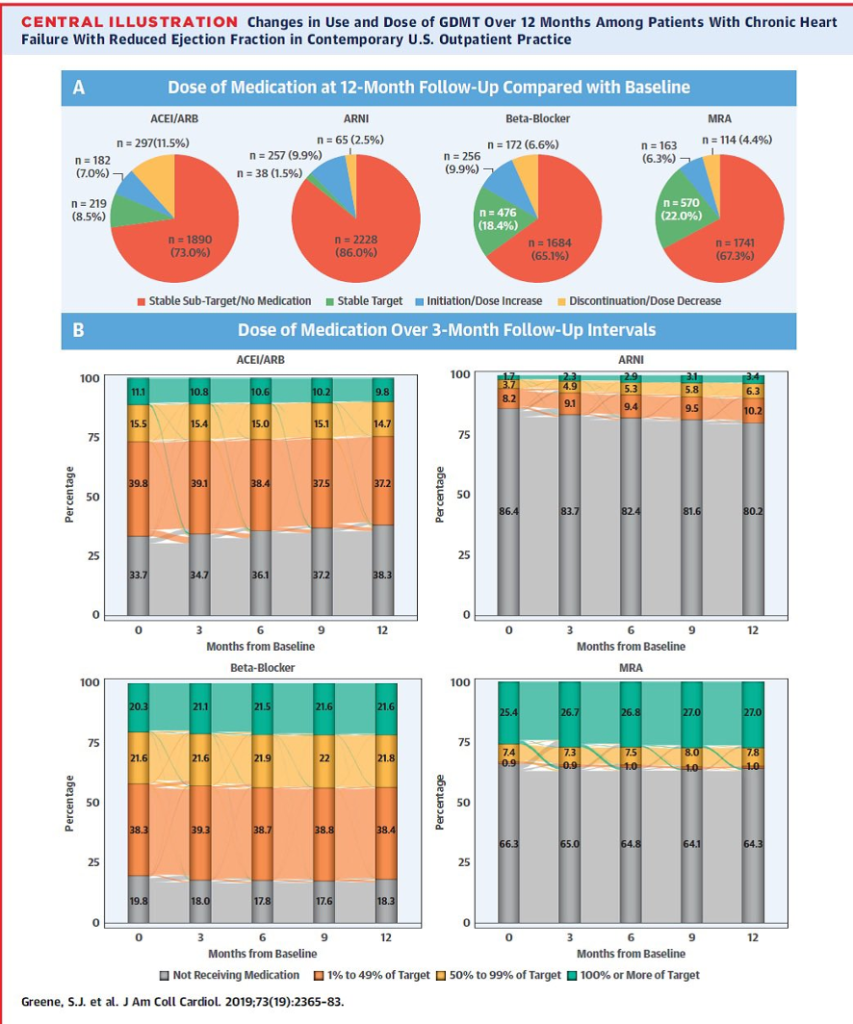
- In multiple studies, protocol-driven titration of GDMT has shown to improve clinical outcomes, yet titration remains poor. The following image from Greene et al. in JACC shows that in contemporary US outpatient practices that GDMT titration is poor with few patients reaching target dosing.
Case #2 Synopsis:
A 43 year-old male with a past medical history of familial dilated cardiomyopathy requiring HVAD placement two years prior now comes in with low flow alarms. He is feeling well otherwise with chronic dyspnea on exertion. A CT chest and abdomen with contrast for showed outflow graft occlusion. Given a TTE showed LV recovery that correlated with invasive hemodynamics, his LVAD was decommissioned. He was tried on a low dose Sacubitril/Valsartan but was unable to tolerate it due to hypotension. He was discharged on carvedilol 3.125mg BID and lisinopril 5mg daily. Over the next 10 months in clinic, his GDMT was titrated to carvedilol 25mg BID, spironolactone 25mg daily and Sacubitril/Valsartan 49-51mg BID.
Takeaways Case #2
- In patients with ventricular assist devices, the differential for low flow alarms includes hypovolemia, arrhythmias, RV failure, cardiac tamponade and inflow cannula obstruction. A careful history, exam (with particular attention to the JVD), and bedside echocardiogram can help differentiate the cause.
- EF recovery occurs in about 5% of patients in large LVAD registries. Favorable prognostic factors for EF recovery include female sex and nonischemic cardiomyopathy of short duration.
- In the TRED-HF trial, patients were randomly assigned to phased withdrawal or continuation of GDMT over 6 months. The primary endpoint was relapse defined as a reduction in LVEF of more than 10% and to less than 50%, an increase in LVEDV by more than 10% and to higher than the normal range, a two-fold rise in NT-pro-BNP and to more than 400 ng/L or clinical evidence of heart failure. While a small trial (51 patients were enrolled), over the first 6 months, 44% of patients assigned to treatment withdrawal met the primary endpoint of relapse compared with none assigned to continue treatment (estimated of event rate 45.7% [95% CI 28.5-67.2]; p=0.0001).
- We still do not have great predictors of relapse, and thus for most patients with HFrecEF, GDMT should continue indefinitely.
References – CardioNerds Rounds: Challenging Cases – Modern Guideline Directed Therapy in Heart Failure with Dr. Randall Starling
- Halliday BP, Wassall R, Lota AS, et al. Withdrawal of pharmacological treatment for heart failure in patients with recovered dilated cardiomyopathy (TRED-HF): an open-label, pilot, randomised trial. Lancet. 2019 Jan 5;393(10166):61-73. doi: 10.1016/S0140-6736(18)32484-X. Epub 2018 Nov 11. PMID: 30429050; PMCID: PMC6319251.
- Greene SJ, Fonarow GC, DeVore AD, et al. Titration of Medical Therapy for Heart Failure With Reduced Ejection Fraction. J Am Coll Cardiol. 2019 May 21;73(19):2365-2383. doi: 10.1016/j.jacc.2019.02.015. Epub 2019 Mar 4. PMID: 30844480; PMCID: PMC7197490.
- McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014 Sep 11;371(11):993-1004. doi: 10.1056/NEJMoa1409077. Epub 2014 Aug 30. PMID: 25176015.
Production Team
 Karan Desai, MD
Karan Desai, MD Natalie Stokes, MD
Natalie Stokes, MD Amit Goyal, MD
Amit Goyal, MD Daniel Ambinder, MD
Daniel Ambinder, MD 





 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast