Cardionerds: A Cardiology Podcast

208. Atrial Fibrillation: Epidemiology, Health Equity, & The Double Paradox with Dr. Larry Jackson
Atrial fibrillation may reach pandemic proportions in the next 2-3 decades. Factors that drive this phenomenon have been studied in predominantly White populations, leading to a significant underrepresentation of certain racial/ethnic groups in atrial fibrillation epidemiological studies. Most atrial fibrillation epidemiology studies suggest that the non-Hispanic Black population has a lower incidence/prevalence of atrial fibrillation, despite a higher risk factor burden (“Afib paradox”). At the same time, non-Hispanic Blacks have worse outcomes compared to the White population and underrepresented populations and women are less likely than White men to receive optimal guideline-based therapies for atrial fibrillation.
In this episode, CardioNerds Dr. Kelly Arps (Co-Chair Atrial Fibrillation series, Cardiology fellow at Duke University), Dr. Colin Blumenthal (Co-Chair Atrial Fibrillation series, CardioNerds Academy House Faculty Leader for House Jones, Cardiology fellow at the University of Pennsylvania), and Dr. Dinu-Valentin Balanescu (CardioNerds Academy Faculty for House Jones, rising internal medicine chief resident at Beaumont Hospital), discuss with Dr. Larry Jackson (cardiac electrophysiologist and Vice Chief of Diversity, Equity, and Inclusion in the Division of Cardiology at Duke University) about atrial fibrillation epidemiology and health equity, challenges and possible solutions to improving diversity in clinical trials, and race/ethnicity/sex/gender differences in the detection, management, and outcomes of atrial fibrillation.
This CardioNerds Atrial Fibrillation series is a multi-institutional collaboration made possible by contributions of stellar fellow leads and expert faculty from several programs, led by series co-chairs, Dr. Kelly Arps and Dr. Colin Blumenthal.
This series is supported by an educational grant from the Bristol Myers Squibb and Pfizer Alliance. All CardioNerds content is planned, produced, and reviewed solely by CardioNerds.
We have collaborated with VCU Health to provide CME. Claim free CME here!
Disclosure: Larry R. Jackson II, MD, MHs, has the following relevant financial relationships:
Advisor or consultant for: Biosense Webster Inc.
Speaker or a member of a speakers bureau for: Biotronik Inc.; Medtronic Inc.
Pearls • Notes • References • Guest Profiles • Production Team

CardioNerds Atrial Fibrillation Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!
Pearls and Quotes – Atrial Fibrillation: Epidemiology, Health Equity, & The Double Paradox
- Atrial fibrillation confers an enormous public health burden. It is estimated that it will reach pandemic proportions over the next 30 years, with potentially 100-180 million people worldwide suffering from this condition.
- Large epidemiological atrial fibrillation registries have very small populations of underrepresented groups. More diverse enrollment in clinical trials is essential and may be obtained by increasing diversity among research staff, principal investigators, and steering committees, and use of mobile/telehealth technologies to remove bias related to differences in presentation. The CardioNerds Clinical Trials Network specifically aims pair equitable trial enrollment with trainee personal and professional development.
- Most atrial fibrillation epidemiology studies suggest that the non-Hispanic Black population has lower incidence/prevalence of atrial fibrillation, despite higher risk factor burden. This “paradox” is likely due to a multifactorial process, with clinical differences, socioeconomic factors, and genetic factors contributing.
- Underrepresented populations are less likely than White patients to receive optimal guideline-based management of atrial fibrillation. Though there is a higher incidence of intracranial bleeding on vitamin K antagonists in this population, they are less likely to receive optimal anticoagulation for stroke prevention with direct oral anticoagulants. Also, despite overall worse outcomes, they are less likely to be prescribed rhythm control strategies or offered catheter-based ablation despite known data with improved outcomes with early rhythm control.
- Gender-based differences in atrial fibrillation epidemiology, management, and outcomes also exist. Compared to men, women have a lower incidence/prevalence of atrial fibrillation but are more likely to be symptomatic. They are also more likely to receive rate instead of rhythm control strategies and suboptimal stroke reduction therapies Overall, women have worse outcomes than men.
“I want to differentiate [equitable care] from equal care. I think this idea of equity means that we have to take into account the myriad of differences that we see between people of different races, ethnicities, genders, sexes, regions, whether they’re citizens or not, whether they’re disabled or not […] and make sure that we’re thinking about those in terms of prescriptions and discussion and communication, and offering our patients therapy, […] it’s not [enough] to offer different people the same therapy because they may have different barriers that may prevent them from uptaking that therapy or utilizing that.”
Dr. Larry Jackson
Notes – Atrial Fibrillation: Epidemiology, Health Equity, & The Double Paradox
Drafted by Dr. Dinu-Valentin Balanescu and reviewed by Dr. Colin Blumenthal.
1. What factors contribute to the atrial fibrillation epidemic and where do we expect to be over the next 20-30 years?
- The current global prevalence of atrial fibrillation is unclear. It is estimated that over the next 30 years, the prevalence of atrial fibrillation may reach pandemic proportions, with potentially 100-180 million people worldwide suffering from this condition.1
- Factors that drive this increase:
- Classic: heart failure, coronary artery disease, hypertension, diabetes, tobacco use, obesity.
- Novel risk factors: obstructive sleep apnea, metabolic syndrome, left ventricular hypertrophy, left atrial enlargement.
- Novel markers (inflammatory, biochemical): B-type natriuretic peptide, CRP.
- Classic: heart failure, coronary artery disease, hypertension, diabetes, tobacco use, obesity.
- Many of the above factors have been determined by studying predominantly White populations.
2. There is conflicting data regarding the incidence of atrial fibrillation across race and ethnicity, with most studies suggesting a higher incidence in the non-Hispanic White population compared to non-Hispanic Black or Hispanic individuals, while some suggest a similar prevalence. How is this discrepancy explained?
- The discrepancy may stem from various rates of clinical detection, rather than incidence or prevalence, of atrial fibrillation between different race/ethnicity groups (“ascertainment bias”).
- Conflicting data persists even when detection is adjusted for. A cohort of the MESA study showed that the prevalence among race and ethnicity was similar when the diagnosis was made using Holter monitor data.2 Data from the ASSERT trial suggest that when using implantable loop recorders, the incidence of atrial fibrillation among the non-Hispanic Black population was lower than a European White population.3
- There is a substantial need for further study on the epidemiology of atrial fibrillation across race/ethnicity.
3. Non-Hispanic Black populations have a higher risk factor burden for atrial fibrillation than White patients, but as described above most studies demonstrate a lower incidence – how is this “paradox” explained?
- The “atrial fibrillation paradox” is a double paradox, as Dr. Jackson explains: despite a higher risk factor burden, non-Hispanic Blacks have a lower incidence/prevalence of atrial fibrillation. At the same time, non-Hispanic blacks have worse outcomes compared to the white population.4
- This is likely due to a multifactorial process, with clinical differences, socioeconomic factors, and genetic factors contributing.5 Specifically:
- Ascertainment bias. Certain racial/ethnic groups may have access issues preventing them from seeking medical attention for rhythm assessment and/or may be less likely to be prescribed rhythm monitors for objective assessment. Additionally, it has been shown that the non-Hispanic Black population has more paroxysmal symptoms, which could lead to difficulties in diagnosis.
- Survival bias. Non-Hispanic Whites have a longer life expectancy compared to underrepresented racial/ethnic groups, which may lead to a greater risk of developing atrial fibrillation over time.
- Genetic/epigenetic differences. Stronger European ancestry within non-Hispanic Blacks is associated with a higher risk of atrial fibrillation. Genome-wide association studies suggest that non-Hispanic Blacks may have protective genes compared to whites.
- Ascertainment bias. Certain racial/ethnic groups may have access issues preventing them from seeking medical attention for rhythm assessment and/or may be less likely to be prescribed rhythm monitors for objective assessment. Additionally, it has been shown that the non-Hispanic Black population has more paroxysmal symptoms, which could lead to difficulties in diagnosis.
4. What are barriers to the diagnosis of atrial fibrillation in understudied populations and how can inclusion in research studies be improved?
- Large epidemiological registries have traditionally included very small proportions of underrepresented groups. A more diverse enrollment in clinical trials is essential.
- Clinical trial participation of marginalized populations may be achieved by:
- Using mobile/telehealth technologies to recruit and follow patients.
- Increasing diversity and heterogeneity among research staff, principal investigators, steering committees, which has been shown to improve study diversity.
- Using mobile/telehealth technologies to recruit and follow patients.
- From a clinical standpoint, barriers may be removed by:
- Educating patients on atrial fibrillation, its complications, its treatments, and its outcomes.
- Involving family and other social communities as part of decision-making support.
- Educating patients on atrial fibrillation, its complications, its treatments, and its outcomes.
5. How are race and ethnicity associated with the workup for atrial fibrillation and the use of specialized diagnostic equipment?
- Clinicians should have a high index of suspicion for atrial fibrillation while understanding the racial/ethnic/gender differences in presentation and management.
- Patients from various racial/ethnic/gender groups may present with different symptoms of atrial fibrillation. For example, non-Hispanic Blacks are more likely to be more symptomatic, but also more paroxysmal. They are also more likely to have a have lower quality of life.6
- If clinical index of suspicion is high, ambulatory monitoring should be pursued.
6. What are the differences in management between White and black patients when it comes to rate versus rhythm control, anticoagulation, and procedures?
- With regards to anticoagulation:
- Black patients are less likely than white patients to be prescribed anticoagulation or, if prescribed, are significantly less likely to be prescribed a direct oral anticoagulant (DOAC).7
- Underrepresented populations have a higher risk of intracranial hemorrhage while on a vitamin K antagonists (VKA) compared to whites. DOACs overall have a lower risk of intracranial hemorrhage and should preferentially be prescribed over VKAs.8
- Pivotal trials comparing DOACs to VKAs have had a very low enrollment of Hispanic and non-Hispanic black populations, so it is possible the benefit is even greater in this population.
- Black patients are less likely than white patients to be prescribed anticoagulation or, if prescribed, are significantly less likely to be prescribed a direct oral anticoagulant (DOAC).7
- With regards to rhythm control strategies:
- Black patients are less likely to receive rhythm control therapies (whether cardioversion, medical, or invasive) and more likely to receive rate control therapy.8
- Black patients have a better response to catheter ablation of atrial fibrillation compared to white patients. This treatment may be preferred in underrepresented populations to improve outcomes compared to medical therapy alone.9
- Black patients are less likely to receive rhythm control therapies (whether cardioversion, medical, or invasive) and more likely to receive rate control therapy.8
7. What are gender-based differences in AF epidemiology and management and are there underlying differences in the electrical conduction system between men and women that affect management decisions?
- Compared to men, women:
- Have a lower incidence and prevalence of atrial fibrillation.
- Are more likely to be symptomatic.
- Are more likely to receive rate control strategies as opposed to rhythm control strategies.
- Are less likely to receive stroke reduction therapies (e.g., anticoagulation or left atrial appendage closure).
- Have worse outcomes: higher risk of stroke, QTc prolongation and torsades de pointes, heart failure, and mortality.10,11
- Have a lower incidence and prevalence of atrial fibrillation.
- These differences may be due to:
- Autonomic differences (especially in the 2nd-5th decades of life).
- Differences in the effects of sex hormones. Estrogen can affect the differential expression of ion channel subunits, ion channel function, inhibits the hERG K channel. Certain sex hormones may also impact action potential duration and alter calcium metabolism.
- Autonomic differences (especially in the 2nd-5th decades of life).
8. Are the differences in the diagnosis, work-up, and treatment of atrial fibrillation among racial/ethnic/gender groups associated with differences in outcomes?
- Underrepresented groups have worse outcomes compared to the White population: higher risk of stroke, heart failure, and mortality.12
- Differences in the management of atrial fibrillation among racial/ethnic/gender groups contribute to these worse outcomes, e.g., lower rates of stroke prevention therapies and rhythm control strategies (patients in sinus rhythm had a 50% reduction in mortality in the AFFIRM trial).9
- The field needs to progress in a way that teaches clinicians to understand barriers in optimal care faced by certain racial/ethnic/gender groups.
9. Dr. Larry Jackson – what makes your heart flutter about electrophysiology and studying health inequity?
- The chance to provide equitable care.
- Equitable care is different from equal care. Equity implies acknowledging the differences between people of different races, ethnicity, genders, regions. These factors should be taken into account when offering therapies to our patients.
- It is not practical to offer different patients the same therapy, as they may have different barriers preventing them from utilizing that therapy.
- Optimal communication and assessment of patient goals with a focus on race/ethnicity/gender leads to better more personalized care.
References – Atrial Fibrillation: Epidemiology, Health Equity, & The Double Paradox
Guest Profiles
 Dr. Paul Cremer
Dr. Paul CremerDr. Larry Jackson is a cardiac electrophysiologist and assistant professor of medicine in the Division of Cardiology at Duke University Medical Center. Dr. Jackson is also an expert researcher, focusing on analyzing racial and ethnic disparities and the impact of social determinants of health on arrhythmia care.
 Dr. Dinu Balanescu
Dr. Dinu BalanescuDr. Dinu Balanescu. Dinu is an internal medicine resident and upcoming chief resident at Beaumont Hospital in Royal Oak, Michigan. He also serves as House Faculty for House Jones in the CardioNerds Academy.
CardioNerds Cardiac Critical Care Production Team
 Karan Desai, MD
Karan Desai, MD Dr. Mark Belkin
Dr. Mark Belkin Dr. Yoav Karpenshif
Dr. Yoav Karpenshif Amit Goyal, MD
Amit Goyal, MD Daniel Ambinder, MD
Daniel Ambinder, MD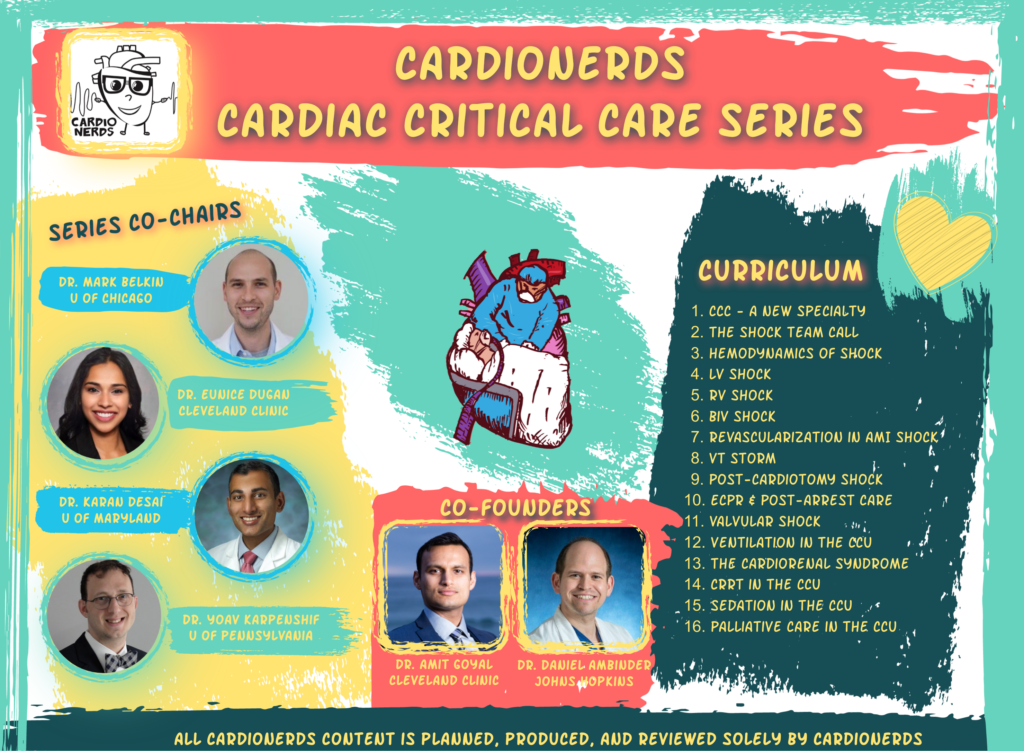






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast