Cardionerds: A Cardiology Podcast

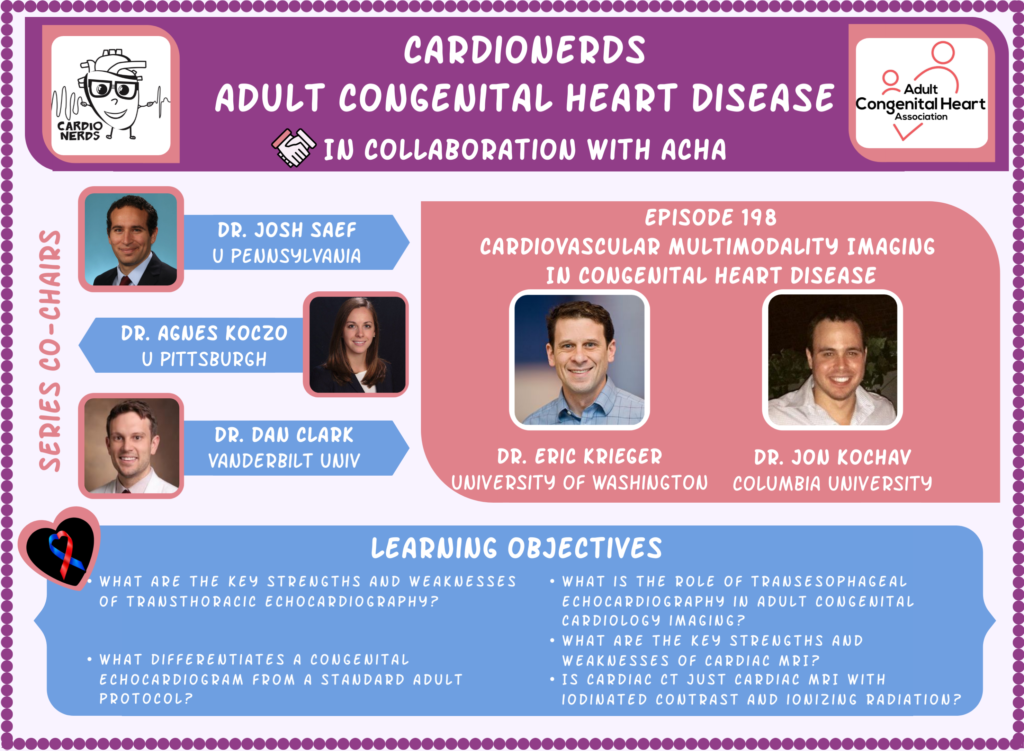
198. ACHD: Cardiovascular Multimodality Imaging in Congenital Heart Disease with Dr. Eric Krieger
CardioNerds (Daniel Ambinder), ACHD series co-chairs, Dr. Josh Saef (ACHD fellow, University of Pennsylvania) Dr. Daniel Clark (ACHD fellow, Vanderbilt University), and ACHD FIT lead Dr. Jon Kochav (Columbia University) join Dr. Eric Krieger (Director of the Seattle Adult Congenital Heart Service and the ACHD Fellowship, University of Washington) to discuss multimodality imaging in congenital heart disease. Audio editing by CardioNerds Academy Intern, Dr. Maryam Barkhordarian. Special introduction to CardioNerds Clinical Trialist Dr. Shiva Patlolla (Baylor University Medical Center).
In this episode we discuss the strengths and weaknesses of the imaging modalities most commonly utilized in the diagnosis and surveillance of patients with ACHD. Specifically, we discuss transthoracic and transesophageal echocardiography, cardiac MRI and cardiac CT. The principles learned are then applied to the evaluation of two patient cases – a patient status post tetralogy of Fallot repair with a transannular patch, and a patient presenting with right ventricular enlargement of undetermined etiology.
The CardioNerds Adult Congenital Heart Disease (ACHD) series provides a comprehensive curriculum to dive deep into the labyrinthine world of congenital heart disease with the aim of empowering every CardioNerd to help improve the lives of people living with congenital heart disease. This series is multi-institutional collaborative project made possible by contributions of stellar fellow leads and expert faculty from several programs, led by series co-chairs, Dr. Josh Saef, Dr. Agnes Koczo, and Dr. Dan Clark.
The CardioNerds Adult Congenital Heart Disease Series is developed in collaboration with the Adult Congenital Heart Association, The CHiP Network, and Heart University. See more
Disclosures: None
Pearls • Notes • References • Guest Profiles • Production Team
CardioNerds Adult Congenital Heart Disease Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!
Pearls – Cardiovascular Multimodality Imaging in Congenital Heart Disease
- Transthoracic echocardiography (TTE) is the first line diagnostic test for the diagnosis and surveillance of congenital heart disease due to widespread availability, near absent contraindications, and ability to perform near comprehensive structural, functional, and hemodynamic assessments in patients for whom imaging windows allow visualization of anatomic areas of interest.
- Transesophageal echocardiography (TEE) use in ACHD patients is primarily focused on similar indications as in acquired cardiovascular disease patients: the assessment of endocarditis, valvular regurgitation/stenosis severity and mechanism, assessment of interatrial communications in the context of stroke, evaluation for left atrial appendage thrombus, and for intraprocedural guidance. When CT or MRI are unavailable or contraindicated, TEE can also be used when transthoracic imaging windows are poor, or when posterior structures (e.g. sinus venosus, atrial baffle) need to be better evaluated.
- Cardiac MRI (CMR) with MR angiography imaging is unencumbered by imaging planes or body habitus and can provide comprehensive high resolution structural and functional imaging of most cardiac and extracardiac structures. Additional key advantages over echocardiography are ability to reproducibly quantify chamber volumes, flow through a region of interest (helpful for quantifying regurgitation or shunt fraction), assess for focal fibrosis via late gadolinium enhancement imaging, and assess the right heart.
- Cardiac CT has superior spatial resolution in a 3D field of view which makes it useful for clarifying anatomic relationships between structures, visualizing small vessels such as coronary arteries or collateral vessels, and assessing patency of larger vessels (e.g branch pulmonary arteries) through metallic stents which may obscure MR imaging. Downsides relative to CMR include requirement of nephrotoxic contrast for imaging of intracardiac/intravascular structures, and while gated images can be obtained throughout the cardiac cycle similarly to CMR, this is particularly costly from an ionizing radiation standpoint.
- When working up an unknown congenital lesion, it is critical to communicate the differential diagnosis when ordering a test so that the imager can protocol the study accordingly. Not all echocardiograms, CT or MRI scans are the same.
Show notes – Cardiovascular Multimodality Imaging in Congenital Heart Disease
What are the key strengths and weaknesses of transthoracic echocardiography?
STRENGTHS:
(1) “Most important ability is availability”: Transthoracic echocardiography is the first line imaging modality in the assessment of patients with congenital heart disease because it is widely available at significantly lower cost with no contraindications or risks to the patient.
(2) Versatility: A wide array of echo approaches can be employed to provide comprehensive structural and physiological data. 2D echo techniques are most useful for visual assessment of cardiac structural abnormalities. Color doppler provides qualitative data regarding flow, and spectral doppler (inclusive of tissue doppler imaging) provides quantitative data defining intracardiac hemodynamics. 3D echo can be applied to optimize imaging planes for valve area planimetry and quantify chamber volumes as well as global contractile function. Strain imaging using 2D speckle tracking techniques can be employed to evaluate regional contractility.
(3) High temporal resolution: High temporal resolution makes echocardiography a superior modality for imaging fast-moving structures (e.g., valvular vegetations or intracardiac masses).
WEAKNESSES:
(1) “You can’t study what you can’t see”: Suboptimal ultrasound penetration can limit transthoracic imaging quality in patients with large body habitus, or patients in the post-operative state. Furthermore, imaging planes are limited by sonographic windows – many anatomic cardiac (e.g., sinus venosus and coronary sinus defects, anomalous coronary arteries) and extracardiac (e.g., aortic dilation/coarctation, anomalous venous return) abnormalities are often incompletely evaluated by echocardiography in adult patients. This is a major limitation as many ACHD conditions are associated with aortopathy and anomalous pulmonary or systemic venous return which may necessitate dedicated cross-sectional imaging. Finally, right ventricular imaging is limited by near field artifact and complex chamber geometry; and similarly anterior structures such as right ventricular to pulmonary arterial conduits are poorly evaluated with transthoracic echocardiography.
What differentiates a congenital echocardiogram from a standard adult protocol?
Congenital echocardiograms obtain more comprehensive anatomic evaluation to visualize structural anomalies that might not be evident in standard imaging planes. Most congenital echo protocols begin with a subcostal short axis and long axis sweep to determine segmental anatomy, visceral and atrial situs, cardiac position, cardiac looping, and arterial situs. Additional views are attempted from the suprasternal position to better characterize major venous and arterial connections and anatomy (bidirectional Glenn, etc.). Sweeps are often obtained between views within the same window to clarify the relationships between anatomic structures and identify abnormalities (e.g. inter-chamber connections) not apparent in the standard imaging planes.
What is the role of transesophageal echocardiography in adult congenital cardiology imaging?
In adult patients with acquired cardiovascular disease, transesophageal echocardiography (TEE) is most commonly employed for the assessment of endocarditis, valvular regurgitation/stenosis severity and mechanism, assessment of interatrial communications in the context of stroke, evaluation for left atrial appendage thrombus, and for intraprocedural guidance. Each of these indications are also commonly encountered in an ACHD population. In congenital cardiology, improved spatial resolution of posterior heart structures can similarly be leveraged to image pathology not well visualized by a transthoracic approach such as for identifying sinus venosus defects, characterizing secundum atrial septal defects to determine feasibility of percutaneous closure, or for assessment of baffle leak on Fontan or atrial switch D-TGA patients. Additionally, TEE increasingly plays a critical role in the perioperative setting (e.g., examining physiology pre- and post-bypass) and for monitoring and guidance of percutaneous interventions in the cardiac catheterization lab.
What are the key strengths and weaknesses of Cardiac MRI?
STRENGTHS:
(1) Unencumbered imaging planes: Unlike echocardiography, for which views are limited by echocardiographic windows, cardiac MRI technicians can prescribe unlimited imaging planes for a more complete coverage of both intracardiac and extracardiac anatomy – particularly with addition of MR angiography. This allows for improved assessment of anterior structures (e.g., the RV, RV-PA conduits), posterior structures (e.g., atrial baffles, sinus venosus or coronary sinus defects), and extracardiac anomalies (e.g., anomalous venous return, aortopathies, pulmonary arterial stenoses), which are usually poorly imaged by echocardiography in adults. Additionally, imaging is generally unaffected by body habitus, and may be used as the primary imaging modality for patients with poor transthoracic windows.
(2) Reproducible volumetric quantification: Cardiac MRI is the gold standard for chamber volume assessment. Chamber volumes are obtained from endocardial contouring of Cine-CMR short axis stacks, allowing for measurements that are independent of geometric assumptions – particularly useful for right ventricular or single ventricle assessments. High inter- and intra-reader reproducibility makes CMR an ideal tool for surveillance of chamber size and function over time, and for assessing response to interventions.
(3) Reproducible flow quantification: Phase contrast pulse sequences are utilized to quantify flow in any imaging plane though a region of interest (e.g., aortic/pulmonary arteries, systemic/pulmonary venous return, branch arteries). This tool can be used in ACHD patients for non-invasive measurement of Qp (pulmonary circuit flow) and Qs (systemic circuit flow) to determine shunt fraction (Qp/Qs), or for quantification of regurgitant volumes in valvular insufficiency (e.g., quantification of pulmonary regurgitation). Measurement of flow velocity across a stenosis can be used to estimate trans-stenotic pressure gradients analogous to echocardiographic spectral doppler – however gradients may be underestimated due to decreased temporal resolution of CMR imaging (peak velocity through region of interest can be missed) or imaging plane not being at the vena contracta (a higher velocity may be obtained at a higher or lower imaging plane).
(4) Tissue characterization: Late gadolinium enhancement CMR can be utilized to assess for myocardial fibrosis – which can be used to identify myocardial infarction in patients with coronary abnormalities, and risk-stratify arrhythmic risk in various conditions (e.g., Tetralogy of Fallot, systemic right ventricle).
(5) 3D evaluation: 3D images can be obtained, allowing for assessment of cardiac structures and their anatomic relations in all planes post image acquisition. Images can be used to produce 3D-printed heart models for surgical planning.
WEAKNESSES:
(1) Not everyone can get an MRI: CMR is contraindicated in patients with ferrous metallic implants. Guidelines now support the use of CMR with both MRI-conditional and legacy cardiac implantable electrical devices – but the need for careful device reprograming and patient monitoring may present logistical hurdles. The risk of nephrogenic systemic fibrosis with the use of gadolinium-based contrast agents in patients with advanced renal disease seems to have been largely mitigated with increased use of cyclic gadolinium-based contrast agents. Moreover, contrast is not required for most of the imaging indications in congenital heart disease. Claustrophobia may be a barrier to a complete CMR study in some patients, as may be intolerance of prescribed breath holds and/or prolonged reclined positioning for patients with heart failure and pulmonary edema.
(2) Reduced image quality in irregular heartbeats: Irregular heart rhythms can impact gating and degrade image quality – a limitation that can be partially mitigated with prospective gating techniques.
(3) The study is only as good as the protocol: MRI technicians prescribe various pulse sequences in specific imaging planes in accordance with the ordered protocol. If there is miscommunication with respect to the clinical question being asked, or the technician is not experienced in imaging patients with congenital heart disease, targeted imaging may not be performed rendering the test nondiagnostic (e.g., a cardiac MRI without MR angiography may miss an anomalous pulmonary vein in a patient with dilated right ventricle).
Is Cardiac CT just Cardiac MRI with iodinated contrast and ionizing radiation?
Cardiac CT has a number of distinct advantages over cardiac MRI – including rapid image acquisition time, greater spatial resolution in a 3-dimensional field of view useful for evaluation of small structures (coronaries, AV malformations, collaterals) and for clarifying anatomic relationships between structures (ideal modality for 3D printing), and ability to be used in patients with cardiac implanted electrical devices without logistic headaches. Gated acquisitions throughout the cardiac cycle can be used to assess ventricular function, although temporal resolution is lesser compared to cardiac MRI and radiation dose for such acquisitions can be substantial. CT angiography also has advantages over MRI in patients for whom prior implanted devices (e.g., stents, coils) obscure the imaging field of interest due to magnetic susceptibility artifact. Ultimately, in young patients who will need multiple imaging studies over the course of their lives, the cumulative ionizing radiation dose associated with cardiac CT is a significant disadvantage. Unlike Echo or CMR, CT imaging does not provide any information on blood flow or cardiac hemodynamics.
Lesion-specific examples:
In these notes, and in the episode, we present two common clinical scenarios in adult congenital heart disease to highlight the importance of a multimodality imaging approach for the diagnosis and surveillance of patients with adult congenital heart disease – (1) assessment of patients with tetralogy of Fallot, and (2) evaluation of patients with right-sided dilatation for shunt. The optimal care of these complex patients often requires appropriate utilization of multiple modalities to leverage the strengths of each.
Lesion
TTE
TEE
Cardiac MRI
Cardiac CT
Tetralogy of Fallot
(1) Routine assessment of RV and LV size and function (2) Routine semiquantitative assessment of pulmonic valve regurgitation (3) Evaluation of PVR/conduit gradients, and RV pressure via tricuspid regurgitation gradient (4) Evaluation of proximal aortic dilation, proximal pulmonary artery branch stenosis (5) Identification of residual intracardiac shunts
(1) Intraoperative management (pre- and post- bypass imaging). (2) Comprehensive echocardiographic evaluation when transthoracic windows are limited, and advanced imaging modalities are unavailable.
(1) Quantitative evaluation of PR severity (phase contrast MRI) when echo-derived severity is inconclusive (2) Serial quantitative assessment of RV volume and ejection fraction to evaluate indications for PVR or conduit replacement in patients with pulmonary insufficiency. (3) MR angiography of aorta and pulmonary artery/branches to assess for dilation or stenosis. (4) Quantitative flow assessment of differential pulmonary arterial blood flow in the setting of branch PA stenosis (phase contrast MRI). (5) Late gadolinium enhancement imaging to assess for RV fibrosis in arrhythmia risk stratification.
(1) Can be used for quantitative RV volume and ejection fraction assessment when CMR is contraindicated at expense of ionizing radiation. (2) Detailed evaluation of aortic and pulmonary arterial anatomy. (3) Detailed evaluation of coronary artery anatomy (e.g., relation of coronary artery to RV to PPA conduit prior to percutaneous valve implantation) (4) Evaluation of aortopulmonary collaterals.
Suspected simple pre-tricuspid shunt lesion (i.e. isolated RV dilatation)
(1) Evaluation of right ventricular size and function. (2) Evaluation of left-sided heart disease as a cause of right-heart disease. (3) Estimation of RV/PA pressure via tricuspid regurgitation gradient to evaluate for suitability of shunt closure (e.g. PA pressure less than 50% of systemic pressure), or alternate explanations of RV dilatation (e.g. primary pulmonary hypertension). (4) Evaluation of the interatrial septum for dropout on 2D images and interatrial flow on color doppler imaging consistent with atrial septal defect (best for visualizing primum and secundum defects). (5) Evaluation of IVC flow for evidence of a scimitar vein (anomalous venous return from R pulmonary veins). (6) L arm bubble study to assess for evidence of coronary sinus defect in patient with dilated and possibly unroofed coronary sinus.
(1) Evaluation for sinus venosus defect in patients with suspected L–>R shunt but no ASD seen on TTE. (2) Evaluation of SVC flow for evidence of partial anomalous venous return from R upper or middle pulmonary veins). (3) Anatomic evaluation of secundum-type defects for candidacy for percutaneous therapy (measurement of defect rim size). (4) Intraprocedural guidance for percutaneous ASD closure.
(1) Quantitative assessment of RV volume and ejection fraction. (2) Non-invasive measurement of shunt fraction (Qp:Qs >1.5 suggests hemodynamically significant shunt) (3) Evaluation for sinus venosus defect in patients with suspected L–>R shunt but no ASD seen on TTE. (4) MR angiography to assess for evidence of anomalous pulmonary venous return (R upper/middle pulmonary veins to SVC, R lower vein or complete R venous drainage to IVC [Scimatar], L venous drainage to innominate [vertical vein] or L venous drainage to coronary sinus).
(1) CTA to assess for evidence of anomalous pulmonary venous return in patients with contraindications to MR angiography.
References
Meet Our Collaborators!
Adult Congenital Heart Association
Founded in 1998, the Adult Congenital Heart Association is an organization begun by and dedicated to supporting individuals and families living with congenital heart disease and advancing the care and treatment available to our community. Our mission is to empower the congenital heart disease community by advancing access to resources and specialized care that improve patient-centered outcomes. Visit their website (https://www.achaheart.org/) for information on their patient advocacy efforts, educational material, and membership for patients and providers
CHiP Network
The CHiP network is a non-profit organization aiming to connect congenital heart professionals around the world. Visit their website (thechipnetwork.org) and become a member to access free high-quality educational material, upcoming news and events, and the fantastic monthly Journal Watch, keeping you up to date with congenital scientific releases. Visit their website (https://thechipnetwork.org/) for more information.

Heart University
Heart University aims to be “the go-to online resource” for e-learning in CHD and paediatric-acquired heart disease. It is a carefully curated open access library of educational material for all providers of care to children and adults with CHD or children with acquired heart disease, whether a trainee or a practicing provider. The site provides free content to a global audience in two broad domains: 1. A comprehensive curriculum of training modules and associated testing for trainees. 2. A curated library of conference and grand rounds recordings for continuing medical education. Learn more at www.heartuniversity.org/

Guest Profiles
 Dr. Yuli Kim
Dr. Yuli KimDr. Eric Krieger is the Associate Director of the University of Washington’s Adult Congenital Heart Disease Program – where he directs the ACHD training program. Dr. Krieger is a multimodality imager – with expertise in applications of cardiac MRI in congenital heart disease.
 Dr. Charlie Jain
Dr. Charlie JainDr. Jon Kochav is an ACHD fellow at Columbia University Medical center. During his general fellowship he spent two research years at the Cardiac MRI lab at Weill Cornell Medical Center.
CardioNerds Adult Congenital Heart Disease Production Team


 Amit Goyal, MD
Amit Goyal, MD Daniel Ambinder, MD
Daniel Ambinder, MD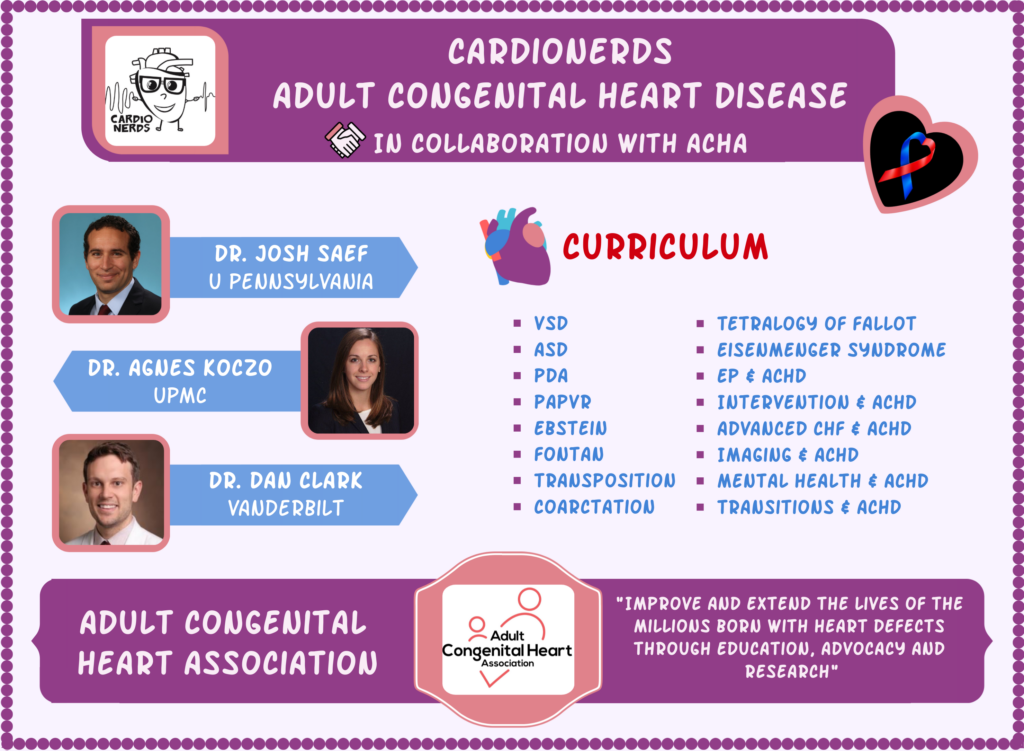






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast