Cardionerds: A Cardiology Podcast

369. Case Report: Apical Obliteration with Biventricular Thrombus – West Virginia University
CardioNerds, Dr. Richard Ferraro and Dr. Dan ambinder join Dr. Li Pang, Dr. Emily Hendricks, and Dr. Bei Jiang from West Virginia University to discuss the following case that features apical obliteration with biventricular thrombus. Dr. Christopher Bianco provides the Expert CardioNerd Perspectives & Review (E-CPR) for this episode. Audio editing by CardioNerds Academy Intern, student doctor Tina Reddy.
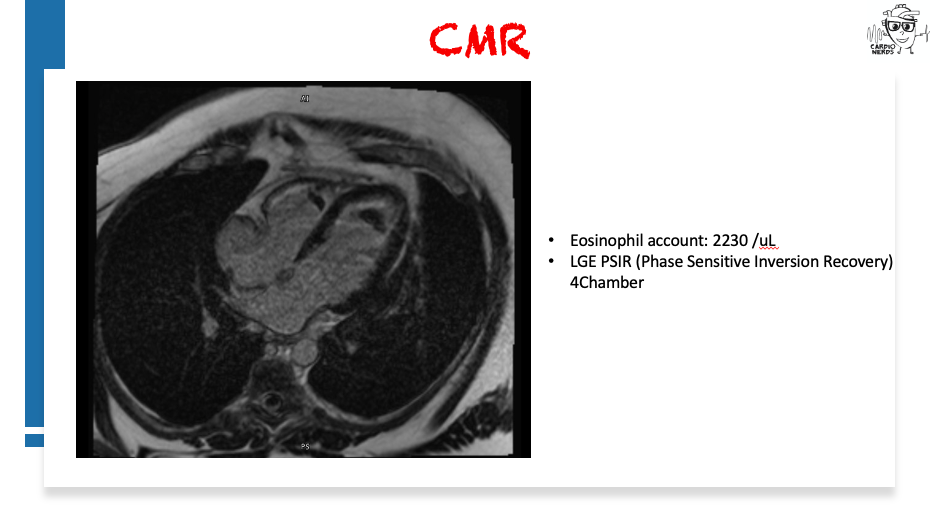
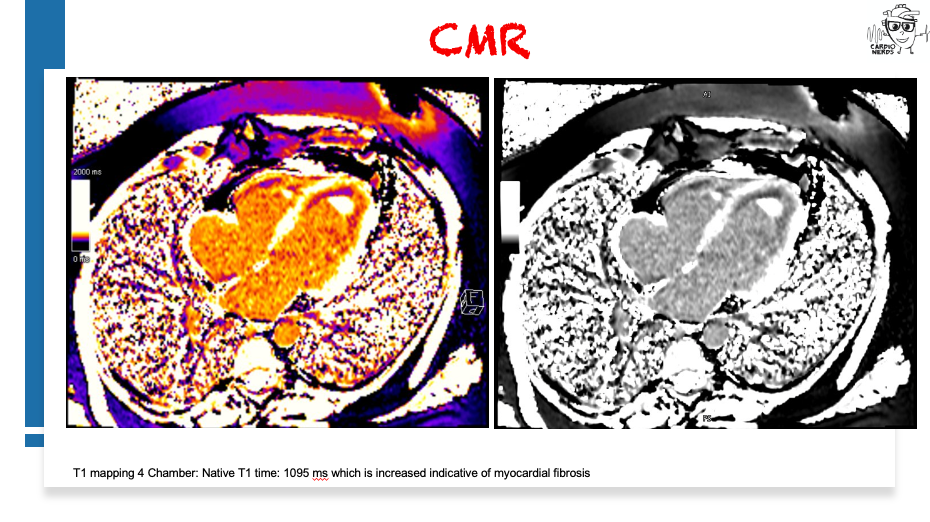
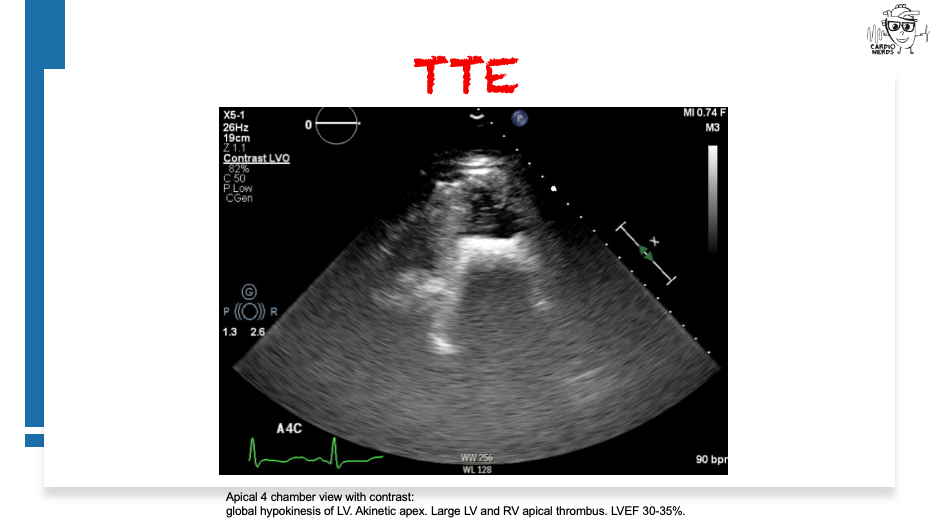
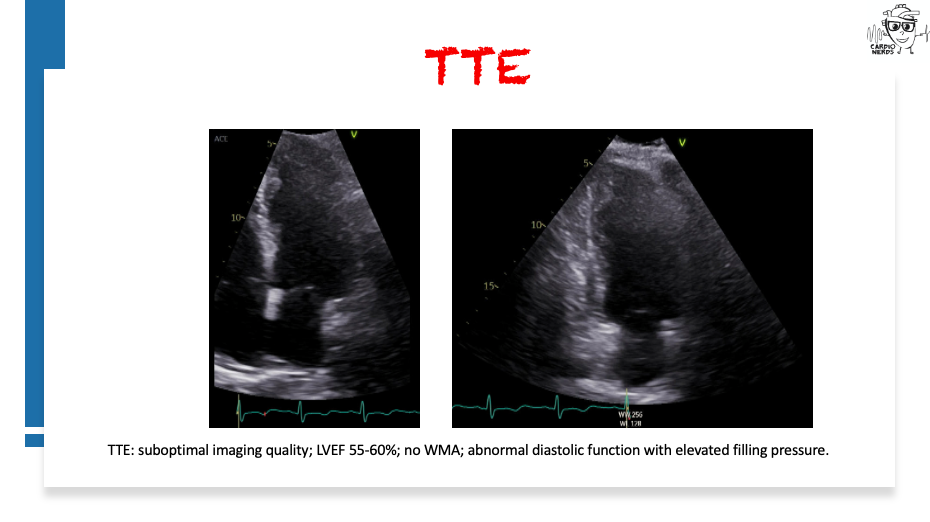
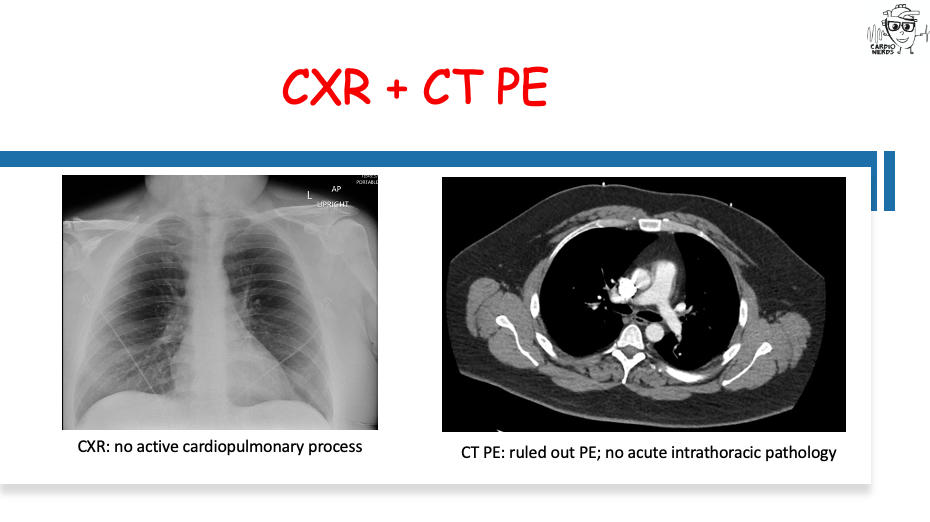
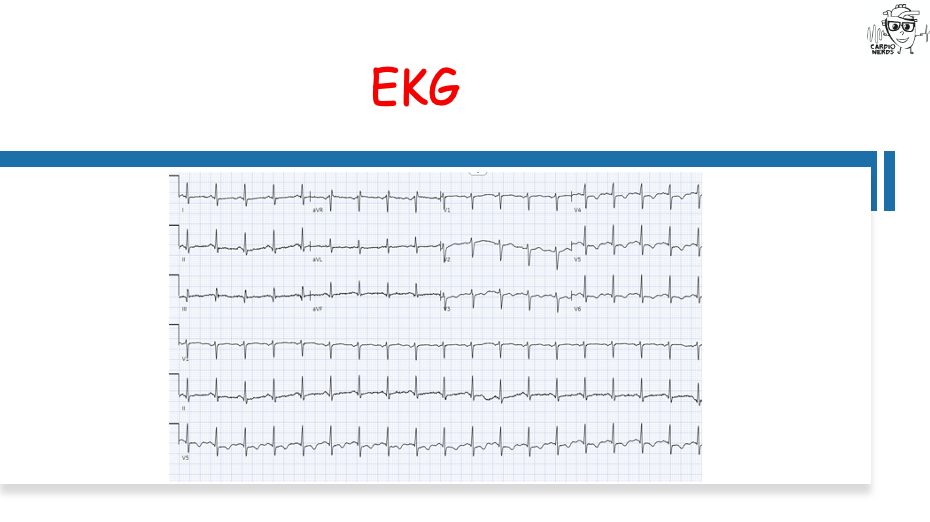
A 37-year-old Caucasian man with a history of tobacco smoking and hypertension who presented with chest pain and elevated troponin was admitted for non-ST elevation myocardial infarction (NSTEMI). Ischemic evaluation with an invasive coronary angiogram was negative. He was treated as NSTEMI and scheduled for outpatient cardiac MRI (CMR). The patient came back 2 months later with right arm weakness and confusion and was found to have an embolic stroke. Labs showed positive troponin with a flat trend and hypereosinophilia. Transthoracic echocardiogram (TTE) showed obliteration of LV and RV apex with thrombus and reduced LV systolic function. CMR was consistent with myocarditis with biventricular thrombus. The patient was started on corticosteroids and warfarin. Hypereosinophilia workup was positive for PDGFRA alpha rearrangement. He was diagnosed with primary hypereosinophila syndrome. Imatinib was initiated. The patient was followed up with the hematology clinic, achieved a complete hematologic response with normalized cell count, and remained free from any cardiovascular event at the 8-month follow-up.
“To study the phenomena of disease without books is to sail an uncharted sea, while to study books without patients is not to go to sea at all.” – Sir William Osler. CardioNerds thank the patients and their loved ones whose stories teach us the Art of Medicine and support our Mission to Democratize Cardiovascular Medicine.
US Cardiology Review is now the official journal of CardioNerds! Submit your manuscript here.

CardioNerds Case Reports Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!
Case Media
Pearls – Apical Obliteration with Biventricular Thrombus
- Cardiac MRI is a valuable test for patients presenting with myocardial infarction with non-obstructive coronary arteries (MINOCA).
- Obliterated apex with apical thrombus on TTE with hypereosinophilia should raise high suspicion for eosinophilic myocarditis.
- Initiation of corticosteroids is the first-line treatment for eosinophilic myocarditis, which is associated with lower mortality in patients with myocarditis. For other potential complications, such as heart failure, intracardiac thrombus, arrhythmia, and pericardial effusion, the standard of care for each disorder is recommended.
- Hypereosinophilia can be seen in parasitic infections, vasculitis, asthma, allergy, hematological malignancies, and as a primary disorder.
Show Notes – Apical Obliteration with Biventricular Thrombus
What is the differential diagnosis for patients with elevated troponin and nonobstructive CAD?
- The occurrence of acute myocardial infarction (AMI) without significant CAD was reported 80 years ago. However, the term MINOCA (myocardial infarction with non-obstructive coronary arteries) has only been used recently to describe these patients. It involves ischemic and nonischemic etiologies. First, overlooked ischemic etiologies need to be ruled out by reconciling the angiogram images such as spontaneous coronary artery dissection (SCAD) and plaque disruption. Intracoronary imaging, such as intravascular ultrasound (IVUS) or optical coherence tomography (OCT), may be applied to evaluate for SCAD and subtypes of plaque disruption when indicated.
- The investigation continues with nonischemic causes such as stress cardiomyopathy, myocarditis, pulmonary embolism, demand ischemia from sepsis, anemia, chest trauma, heart failure exacerbation, arrhythmia, and stroke.
- The diagnosis of MINOCA is established when it fulfills the following criteria: First, it is AMI by the Fourth Universal Definition; Second, less than 50% of stenotic lesion on angiogram; Third, there is no alternate diagnosis. MINOCA etiologies include coronary artery spasms and microvascular dysfunction.
- It is recommended to perform CMR in all MINOCA patients without an obvious underlying cause.
What are the common causes of LV thrombus?
- The incidence of LV thrombus has been reported between 4-39% after anterior MI. The temporal incidence has been decreasing. It is also commonly seen in dilated cardiomyopathy with an incidence of 2-36%.
- The pathophysiology of intracardiac thrombus formation obeys Virchow’s triad rule, which states that endocardial injury, hypercoagulability/inflammation, and stasis lead to thrombogenesis.
- Other etiologies of LV thrombus include eosinophilic myocarditis and LV noncompaction.
What are the characteristic echocardiographic and CMR findings of eosinophilic myocarditis (EM)?
- During the acute necrotic stage, there is increased subendocardial echogenicity, wall thickening, impaired regional wall motion, and pericardial effusion; there is edema without fibrosis on CMR.
- During the thrombotic stage, intracardiac thrombus is often detected in the ventricles on TTE; on CMR, there is endomyocardial involvement and intracardiac thrombus.
- During the fibrotic stage, in addition to the cumulative findings from previous stages, restrictive physiology, valvular thickening, and restricted motion can occur on TTE; on CMR, endomyocardial fibrosis with LGE is present.
What is the management for eosinophilic myocarditis (EM)?
- Two aspects must be considered in the treatment of eosinophilic myocarditis: the management of acute cardiac conditions and the treatment of underlying causes.
- Corticosteroids are the first-line treatment for EM. A meta-analysis of 179 cases showed that steroid use is associated with a lower mortality rate. No clinical trial data are available for the treatment of eosinophilic myocarditis. The dose and duration of corticosteroids in each individual case can be different.
- For intracardiac thrombus, vitamin K antagonists (VKAs) are the drugs of choice. Complete gradual resolution of intracardiac thrombus with VKA in eosinophilic myocarditis was reported at the 18-month follow-up. The INR target was 2-3. Emerging data showed the noninferiority of using DOAC for LV thrombus compared to warfarin as an alternative for stroke prevention. There is an increased risk of stroke in patients on VKA but with subtherapeutic INR levels. The guidelines recommend DOAC as a reasonable alternative to VKA to treat LV thrombus.
- For other potential complications such as heart failure, intracardiac thrombus, arrhythmia, and pericardial effusion, the standard of care for each complication is recommended. There is no large data to suggest a specific approach in eosinophilic myocarditis. It has been reported to achieve full recovery with GDMT in addition to treating the underlying cause in a case report of eosinophilic myocarditis with severely reduced LV systolic function.
What is hypereosinophilic syndrome (HES)?
- HES is pleomorphic in clinical presentation and can be idiopathic or associated with a variety of underlying conditions, including allergic, rheumatologic, infectious, and neoplastic disorders.
- There are 4 groups. In primary HES, the hypereosinophilia is driven by a clonal process in stem cell or myeloid lineage. Patients usually present with a myeloid neoplasm and myeloid proliferative disorder. Besides eosinophilia, they may have other cytopenias, blasts, or dysplastic cells in peripheral blood. They can present with constitutional symptoms or hepatosplenomegaly. Some of these patients have disease-defining mutations or chromosome translocation. They require treatment for their underlying hematologic condition. Secondary HES usually have polyclonal eosinophilia secondary to some stimulus. The stimulus may be infections, rheumatology conditions, solid tumors, and lymphoid neoplasm. The underlying condition increases eosinophilic cytokines leading to an increase in eosinophil production. The third group is familial HES results from certain genetic factors. If no cause of HES can be identified, they fall into the category of idiopathic HES.
- Patients with HES secondary to myeloid and lymphoid disorders need to follow up with a hematology specialist.
References – Apical Obliteration with Biventricular Thrombus
- Bondue A, Carpentier C, Roufosse F. Hypereosinophilic syndrome: considerations for the cardiologist. Heart 2022;108:164-171.
- Merlo M, Gagno G, Baritussio A et al. Clinical application of CMR in cardiomyopathies: evolving concepts and techniques : A position paper of myocardial and pericardial diseases and cardiac magnetic resonance working groups of Italian society of cardiology. Heart Fail Rev 2023;28:77-95.
- Murthy SB. Troponin Elevation After Ischemic Stroke and Future Cardiovascular Risk: Is the Heart in the Right Place? Journal of the American Heart Association 2021;10:e021474.
- Dhaliwal JSS, Ansari SA, Ghosh S, Chitkara A, Khizer U. Duet of Death: Biventricular Thrombus in a Methamphetamine User. Cureus 2023;15:e39917.
- Levine GN, McEvoy JW, Fang JC et al. Management of Patients at Risk for and With Left Ventricular Thrombus: A Scientific Statement From the American Heart Association. Circulation 2022;146:e205-e223.
- Parrillo JE. Heart Disease and the Eosinophil. New England Journal of Medicine 1990;323:1560-1561.
- Wright BL, Leiferman KM, Gleich GJ. Eosinophil Granule Protein Localization in Eosinophilic Endomyocardial Disease. New England Journal of Medicine 2011;365:187-188.
- Polte CL, Bobbio E, Bollano E et al. Cardiovascular Magnetic Resonance in Myocarditis. Diagnostics 2022;12:399.
- Ammirati E, Frigerio M, Adler ED et al. Management of Acute Myocarditis and Chronic Inflammatory Cardiomyopathy: An Expert Consensus Document. Circ Heart Fail 2020;13:e007405.
- Ito S, Isotani A, Yamaji K, Ando K. Follow-up magnetic resonance imaging of Löffler endocarditis: a case report. Eur Heart J Case Rep 2020;4:1-4.
- Miller T, Gabriel A, Bianco C, Hamirani Yasmin S. ACUTE EOSINOPHILIC MYOCARDITIS: AN ATYPICAL PRESENTATION DIAGNOSED BY COMBINED CARDIAC MAGNETIC RESONANCE IMAGING AND ENDOMYOCARDIAL BIOPSY WITH FULL RECOVERY. Journal of the American College of Cardiology 2022;79:2298-2298.






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast