Defocus Media Podcast Network

Revolutionary Glaucoma Imaging: Heidelberg Engineering’s Glaucoma Module Premium Edition
In this episode, our glaucoma expert host, Dr. Chris Lievens, brings his unique flair to the table as he interviews esteemed experts in the field to discuss Heidelberg Engineering’s Glaucoma Module Premium Edition. Get ready to be enthralled as Dr. Swarup Swaminathan from the Bascom Palmer Institute and Dr. Jim Williamson of the Memphis VA Medical Center share their invaluable insights. Together, they will unravel the intricacies of Heidelberg Engineering’s Glaucoma Module Premium Edition, showcasing how this revolutionary technology is transforming the eye care landscape. Whether you’re a seasoned practitioner or fascinated by groundbreaking medical advancements, this podcast promises to engage, enlighten, and inspire. Tune in for a dynamic exploration of glaucoma care like never before!
In Partnership with Heidelberg Engineering
 What’s Covered:
What’s Covered: - Introduction to Heidelberg Engineering’s Technology and Guest Experts
- Challenges in Glaucoma Identification and Management in 2023
- Advantages of Glaucoma Module Premium Edition in Glaucoma Management
- The Role of the Anatomic Positioning System (APS) in Glaucoma Imaging
- Understanding and Utilizing the Hood Report in Glaucoma Management
- Navigating Color Coding in Ophthalmic Imaging
Dr. Chris Lievens:
Hello everyone. Thank you for tuning in to the Four-Eyed Professor podcast. In this episode, we will discuss Heidelberg Engineering’s technology, focusing on the Glaucoma Module Premium Edition and its benefits for patients. Please note that the opinions expressed by my guests and me do not necessarily reflect those of Heidelberg Engineering. Today, I am excited to have two expert colleagues, Dr. Swarup Swaminathan and Dr. Jim Williamson, who will share their insights with us.
Dr. Swarup Swaminathan:
Thank you for the opportunity to be here. I’m an assistant professor of ophthalmology at the Bascom Palmer Institute at the University of Miami. I’ve been fortunate to work here for the past four years, completing my residency and fellowship training at Duke University. My practice primarily focuses on glaucoma and cataract patients, and I’m also heavily involved in clinical informatics research, especially in statistical modeling for glaucoma progression. I’m eager to discuss our experiences with Heidelberg’s Spectralis.
Dr. Chris Lievens:
Wonderful, Jim. Could you tell us about yourself?
Dr. Jim Williamson:
Absolutely. I’m based in Memphis, Tennessee, where I’ve worked for 22 years as the residency supervisor at the Memphis VA Medical Center. Like Swaroop, I have extensive experience with Heidelberg’s technology. I look forward to discussing their offerings in more detail.
Challenges in Glaucoma Identification and Management in 2023
Dr. Chris Lievens:
Excellent. So, moving beyond the important but extensive topic of patient compliance, let’s discuss the challenges we face in 2023 regarding the identification, monitoring, and management of glaucoma. Swaroop or Jim, would you like to start?
Dr. Jim Williamson:
Identifying glaucoma is complex, especially when training residents and students. Often, patients come to our clinic with an outside diagnosis of glaucoma, but there are many intricacies that can lead to misdiagnosis. The Glaucoma Module Premium Edition (GMP) offers tools that help differentiate true glaucoma cases from other conditions. This differentiation is crucial. Compliance is another ongoing issue, and I’m particularly interested in discussing surgical mixed procedures as an alternative to eye drops, offering a more permanent solution for our patients.
Dr. Swarup Swaminathan:
Jim makes some excellent points. Educating trainees that glaucoma is a progressive condition is vital. We frequently receive referrals for glaucoma at our tertiary care center, but many cases turn out to be non-progressive anomalies, like scarring, which affect OCT scans or visual fields. For instance, I had a patient who had been on three different eye drops for 15 years. Upon examination, we realized her condition was not glaucoma, and discontinuing the drops significantly improved her quality of life. It’s important to understand and identify these non-progressive conditions. One method I find particularly effective is showing patients their scans on the Spectralis, which helps them understand the areas of concern in their retina.
Advantages of Glaucoma Module Premium Edition in Glaucoma Management
Dr. Chris Lievens:
What other advantages do imaging techniques offer in managing glaucoma, particularly in identifying early cases or subtle progression?
Dr. Swarup Swaminathan:
Absolutely. The B-scans are incredibly useful for patient education. The feature in the Spectralis that allows us to compare circle scans from different times is particularly beneficial. We can demonstrate to patients how their condition has changed over time. The 61-line scan in the Glaucoma Module Premium Edition (GMPE) is also essential. It provides a wealth of information, not just about the optic nerve head but also about potential co-existing pathologies like dry AMD.
Discovering subtle changes, such as converting to wet AMD, can be critical. Similarly, when I notice an area of loss or subtle progression, I use the posterior pole report to compare macula scans over time. This is powerful for both diagnosis and patient communication, as we can show them specific areas of change in a way that’s easy to understand.
Dr. Jim Williamson:
I agree, especially regarding the Magnum scan. It’s impressive how well it segments the ganglion cell layer, providing valuable information. As Swarup mentioned, the ability to toggle between scans is a significant advantage. Also, multimodal imaging, such as blue autofluorescence, is crucial. It allows us to demonstrate retinal nerve fiber layer (RNFL) defects in patients by comparing their scans with those of healthy controls. This visual representation can be very effective in helping patients understand their condition.
The Role of the Anatomic Positioning System (APS) in Glaucoma Imaging
Dr. Chris Lievens:
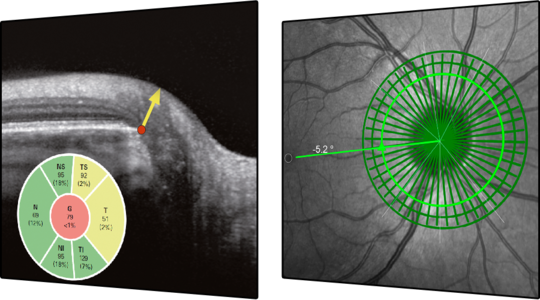
The GMPE’s Anatomic Positioning System (APS) is another fascinating feature. Since not everyone’s optic nerve is oriented perfectly, like in a textbook, the APS adjusts for torsional changes in the optic nerve insertion. This adjustment ensures that we are comparing like with like in our retinal layer segmentations and posterior pole asymmetry analyses. The system automatically compensates for these variations, providing consistent, quality information. Have you also noticed the benefits of this feature in your practice?
Dr. Jim Williamson:
Yes, the APS is a significant advancement. Early on, we noticed the symmetrical RNFL shifts that could occur in scans. However, with the GMP, these shifts are much less common, providing a more accurate representation of the patient’s condition. This advancement is particularly noticeable when comparing older RNFL scans to those obtained with the GMP. The accuracy and consistency of the GMP scans are vital for effective diagnosis and management of glaucoma.
Understanding and Utilizing the Hood Report in Glaucoma Management
Dr. Jim Williamson:
I find the Hood report to be a valuable tool, albeit in a different way from Swarup. It’s particularly useful for patient education, as it provides a visual representation that patients can understand more easily. The overlay of visual field points with RNFL or GCL data can be incredibly informative. When there’s a focal loss in the RNFL, it often corresponds directly to a scotoma in the visual field, and seeing this correlation can be quite enlightening for patients.
Regarding daily use, I agree with Swarup that it might not be necessary for every case. However, for complex cases or when there’s an unusual pattern of loss, the Hood report can offer deeper insights. It helps understand the relationship between structural and functional changes, which is crucial in managing glaucoma.
While it may be a bit advanced for trainees, I believe it’s important to expose them to these tools. The more they understand and can use these advanced imaging techniques, the better equipped they’ll be in their future practices. As for the ISNT rule, it’s a classic approach that I still use as a foundational concept, but these new technologies, like the Hood report, provide a more nuanced view that can be very beneficial.
Dr. Chris Lievens:
It’s interesting to see how both of you utilize these tools differently. Swarup focuses more on the practicality and ease of communication with patients and trainees, while Jim sees the value in the detailed insights provided by the Hood report for complex cases and patient education. The evolution from traditional rules like ISNT to more advanced imaging interpretations underscores how technology enhances our understanding and management of glaucoma. It’s a balance between the simplicity of traditional methods and the depth of information offered by newer technologies.
Navigating Color Coding in Ophthalmic Imaging
Dr. Chris Lievens:
Navigating the reliance on color coding in ophthalmic imaging is a complex and nuanced issue. It’s important to train both students and clinicians to look beyond the red, yellow, and green color codes and analyze the data in its entirety.
Dr. Jim Williamson:
The biggest challenge is understanding that the color coding is based on a reference database and doesn’t provide a conclusive diagnosis. It’s essential to interpret these colors within the context of each patient’s unique ocular profile. Misinterpretations, especially due to refractive errors, can lead to incorrect diagnoses. Emphasizing trend analysis and considering multiple factors in optic nerve evaluation are key.
Dr. Swarup Swaminathan:
Indeed, the reference database is just a starting point. Its limitations, such as refractive biases, must be recognized. In my own experience as a highly myopic individual, my scans showed red areas due to anatomical variations, not pathology. It’s crucial to focus on the overall topography and not just the colors. The TISNet plot, for instance, provides a wealth of information beyond the color coding. It’s also important to remember that being in the ‘green’ range doesn’t necessarily mean there’s no progression. Educating trainees on these subtleties is vital for accurate diagnosis and patient management.
Dr. Chris Lievens:
This discussion underscores the importance of comprehensive training and a deeper understanding of ophthalmic imaging interpretations. It’s not just about the colors but the story behind them, integrating various clinical factors and understanding the patient’s unique ocular characteristics.
Dr. Swarup Swaminathan:
Jim’s point about the selective use of scans is spot on. While I don’t frequently use the BMO scans, they are invaluable in certain situations. I recall instances where patients had unusual optic nerves with RNFL loss, and instead of needing additional tests like autofluorescence or B-scans, the GMP allowed us to discover buried drusen, explaining the observed anomalies. The key is to have that data available when you need it. Although not every patient requires such detailed examination, having the option to conduct these scans is immensely beneficial. It’s about having the flexibility to delve deeper into the optic nerve’s health when necessary.
Dr. Chris Lievens:
That’s a significant point. The versatility of the GMP is remarkable. It allows for customized progression tracking in various parts of the optic nerve and surrounding tissues. This flexibility is vital, enabling us to monitor specific areas over time, tailoring our approach to each patient’s unique condition. Selecting and tracking any part of the nerve or tissue over repeated scans enhances our diagnostic and management capabilities. This feature of the GMP is one of its most powerful attributes, offering personalized and precise care for our patients.






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast