Core EM - Emergency Medicine Podcast

Episode 194: Nitrous Oxide Toxicity

We review Nitrous Oxide Toxicity: Symptoms, diagnosis, and treatment overview
Hosts:
Stefanie Biondi, MD
Brian Gilberti, MD
https://media.blubrry.com/coreem/content.blubrry.com/coreem/Nitrous_Oxide_Toxicity.mp3
Download
Leave a Comment
Tags: Toxicology
Show Notes
Patient Case Illustration
- Hypothetical case: 21-year-old male with no previous medical history, experiencing a month of progressively worsening numbness, tingling, and weakness. Initially starting in his toes and spreading to his hips, and later involving his hands, the symptoms eventually escalated to the point of immobilization. Despite initially denying drug use, the patient admitted to using 40-60 canisters of nitrous oxide (whippets) every weekend for the last three months.
Background and Recreational Use of Nitrous Oxide
- Nitrous oxide, a colorless, odorless gas with anesthetic properties.
- Synthesized in the 18th century.
- Its initial medical purpose expanded into recreational use due to its euphoric effects.
- Resurgence as a recreational drug during the COVID-19 lockdowns.
- Accessibility and legal status.
Public Misconceptions and Health Consequences
- There are widespread misconceptions about nitrous oxide
- Particularly the belief in its safety and lack of long-term health risks.
- Contrary to popular belief, frequent use of nitrous oxide can lead to significant, sometimes irreversible, health issues.
- Particularly the belief in its safety and lack of long-term health risks.
Neurological Examination and Diagnosis
- Key components of the examination include assessing strength, sensation, cranial nerves, and proprioception, with specific abnormalities such as symmetrically decreased strength in a stocking-glove pattern, upgoing Babinski reflex, and positive Romberg sign being indicative of potential toxicity.
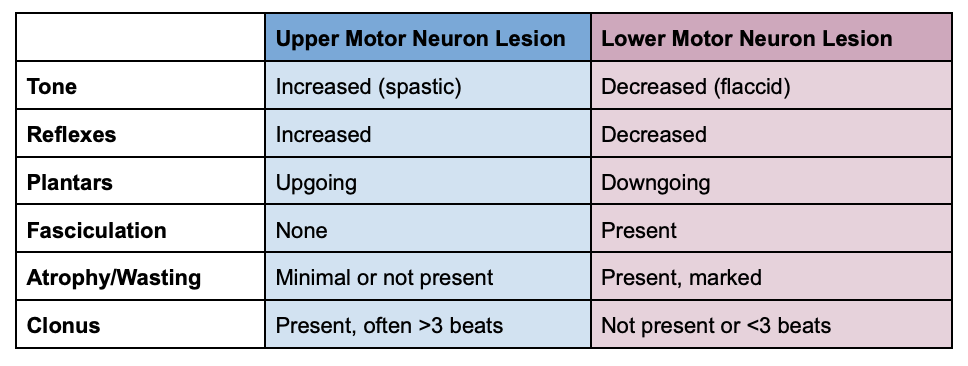
Physical Exam Findings: Upper vs Lower Motor Neuron Lesions
Localize the Lesion- Differential Diagnoses for Extremity Weakness
Localize the Lesion- Differential Diagnoses for Extremity Weakness
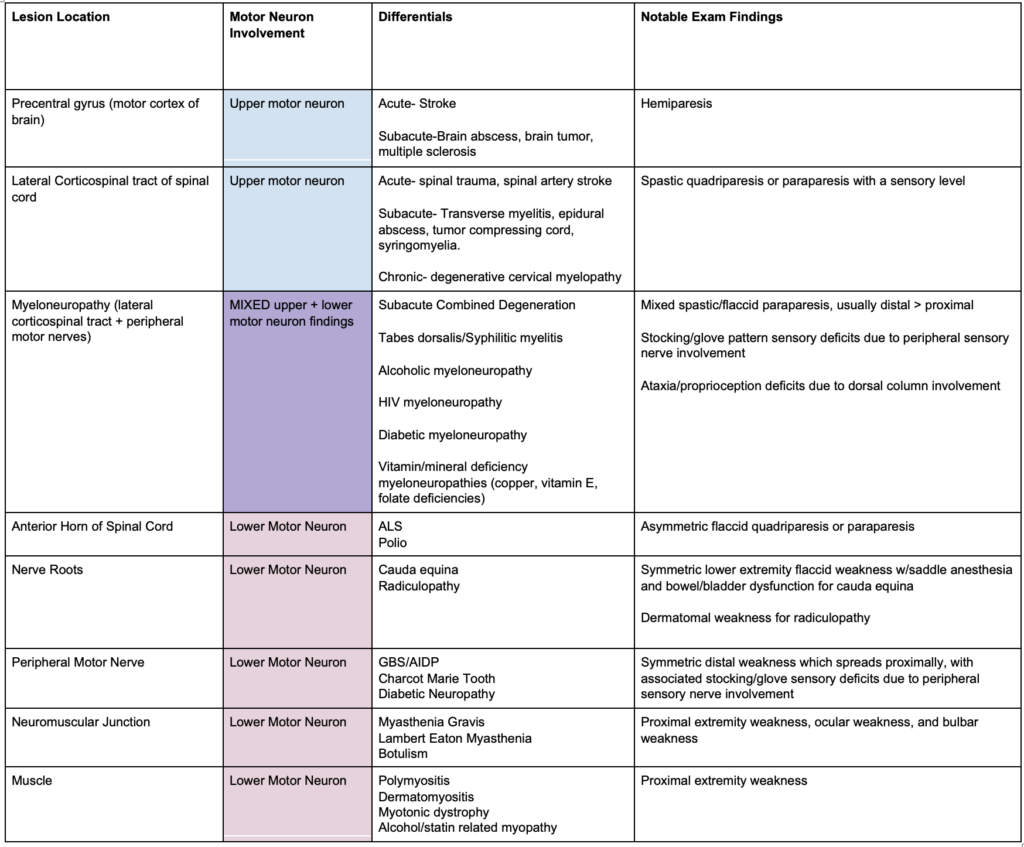
Localize the Lesion- Differential Diagnoses for Extremity Weakness
MRI Findings and Subacute Combined Degeneration
- The MRI displayed symmetric high signal intensity in the dorsal columns, a diagnostic feature identified as the inverted V sign or inverted rabbit ear sign.
- Significance of the Inverted V Sign: This MRI sign is pathognomonic for subacute combined degeneration, indicating it is a distinct marker for this condition.
- T2 Weighted Axial Images: The inverted V sign is observed in T2 weighted axial MRI images, which are used to evaluate the presence and extent of demyelination within the spinal cord.
- Interpretation of Hyperintense Signals: Hyperintense signals on T2 weighted images generally indicate demyelination, where the protective myelin sheath around nerve fibers is damaged or destroyed.
- Anatomical Location: The dorsal columns, located anatomically dorsal (toward the back) within the spinal cord, will appear toward the bottom of the screen in an axial (cross-sectional) view on the MRI.
- Demyelination Appearance: Demyelination in the dorsal columns, typically situated in the thoracic spine, manifests as an upside-down V shape on the MRI, correlating with the described inverted V or rabbit ear sign.
Pathophysiology of SCD due to Nitrous Oxide
- Nitrous Oxide’s Effect on Vitamin B12: Nitrous oxide inactivates vitamin B12 by oxidizing a cobalt component within the molecule, rendering the vitamin functionally ineffective despite adequate consumption and absorption.
- Impact on Methionine Synthase: The oxidation of vitamin B12 by N2O prevents it from activating methionine synthase, an enzyme critical for important biochemical processes.
- Folate to Tetrahydrofolate Conversion: Inactive methionine synthase cannot convert folate into tetrahydrofolate, which is necessary for DNA synthesis. This disruption can lead to megaloblastic anemia, a condition associated with N2O-induced subacute combined degeneration.
- Conversion of Homocysteine to Methionine: Methionine synthase is also responsible for converting homocysteine to methionine. Methionine is essential for the maintenance of myelin integrity, the protective sheath around nerve fibers.
- Demyelination and Neurological Symptoms: The inability to maintain myelin integrity due to disrupted methionine production leads to the demyelination of dorsal columns and peripheral motor/sensory nerves, characteristic of N2O-SCD.
- Normal B12 Levels with Functional Deficiency: Blood levels of vitamin B12 can appear normal in individuals affected by N2O exposure, as the issue lies in the vitamin’s inactivation rather than its absence, creating a functional deficiency.
- Diagnosis of N2O-SCD: To diagnose N2O-induced SCD, healthcare providers need to check for elevated levels of methylmalonic acid and homocysteine. These substances are typically metabolized with the help of vitamin B12, and their elevated levels indicate a functional deficiency of B12 due to N2O exposure.
Treatment and Management
- Lack of Standardized Treatment: There is no universally accepted treatment protocol for N2O induced SCD, but common practices exist based on neurologist recommendations.
- B12 Injection Protocol: A common approach involves administering vitamin B12 injections daily or every other day until there is noticeable improvement in symptoms. Once symptoms start to improve, the frequency of injections can be reduced to once a week.
- Importance of Abstinence from N2O: For recovery to be possible, it is crucial that the patient completely abstains from using whippets (recreational N2O canisters). Continuing to use N2O can inactivate the administered vitamin B12, undermining the treatment efforts.
- Recovery Process: Recovery from N2O induced SCD is typically slow and may not be complete. While remyelination and neurological function can gradually improve, the process is lengthy and may not fully return to baseline.
- Recovery Statistics: Approximately 80% of individuals with N2O-SCD experience some improvement after a year of consistent B12 treatment. However, only between 10% and 20% of patients fully recover to their pre-condition baseline.
- Risk Factors and Prevalence: The risk of developing SCD correlates with the frequency and quantity of N2O use. About 3.4% of individuals who use whippets will develop SCD, with the risk increasing to 8.5% among those who use more than 100 canisters per session. The case in point involved a patient using 20-40 canisters per session.
- Increased Risk with Preexisting Conditions: Individuals who already have a vitamin B12 deficiency are at a greater risk of experiencing SCD symptoms, even with minimal use of whippets. This highlights the importance of understanding individual health conditions and potential vulnerabilities when assessing risk.
Conclusion and Preventive Measures
- Providers should be vigilant in screening for nitrous oxide use among patients presenting with unexplained neurological symptoms. The goal is to enhance early detection and treatment of N2O-induced SCD and to educate patients on the potential long-term health consequences of recreational nitrous oxide use.
References
- Neurology. Mumenthaler M, Mattle H, Taub E, ed. 4th Edition. Stuttgart: Thieme; 2003. doi:10.1055/b-005-148905
- Zayia LC, Tadi P. Neuroanatomy, Motor Neuron. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554616/
- Khin-Htun S, Tan H, Aung T. “Approach to a Patient With Weakness” 2021 Feb 15. Youtube. https://www.youtube.com/watch?v=3WQvtCuC4Fo&t=922s
- Bhattacharyya S.Spinal Cord Disorders: Myelopathy, The American Journal of Medicine, Volume 131, Issue 11, 2018, Pages 1293-1297, ISSN 0002-9343,https://doi.org/10.1016/j.amjmed.2018.03.009.
- Garg RK, Malhotra HS, Kumar N. Approach to a case of myeloneuropathy. Ann Indian Acad Neurol. 2016 Apr-Jun;19(2):183-7. doi: 10.4103/0972-2327.182303. PMID: 27293327; PMCID: PMC4888679.
- Lim PAC. Transverse Myelitis. Essentials of Physical Medicine and Rehabilitation. 2020:952–9. doi: 10.1016/B978-0-323-54947-9.00162-0. Epub 2019 Apr 17. PMCID: PMC7151963.
- Jayarangaiah A, Lui F, Theetha Kariyanna P. Lambert-Eaton Myasthenic Syndrome. [Updated 2023 Oct 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507891/
- Nguyen TP, Taylor RS. Guillain-Barre Syndrome. [Updated 2023 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532254/
- Froese DS, Fowler B, Baumgartner MR. Vitamin B12 , folate, and the methionine remethylation cycle-biochemistry, pathways, and regulation. J Inherit Metab Dis. 2019 Jul;42(4):673-685. doi: 10.1002/jimd.12009. Epub 2019 Jan 28. PMID: 30693532.
- Guo CJ, S. Kaufman B. Inhalational Anesthetics. In: Nelson LS, Howland M, Lewin NA, Smith SW, Goldfrank LR, Hoffman RS. eds. Goldfrank’s Toxicologic Emergencies, 11e. McGraw-Hill Education; 2019. Accessed February 27, 2024. https://accessemergencymedicine-mhmedical-com.ezproxy.med.nyu.edu/content.aspx?bookid=2569§ionid=210274345
- Lin JP, Gao SY, Lin CC. The Clinical Presentations of Nitrous Oxide Users in an Emergency Department. Toxics. 2022 Feb 26;10(3):112. doi: 10.3390/toxics10030112. PMID: 35324737; PMCID: PMC8950993.
- Qudsiya Z, De Jesus O. Subacute Combined Degeneration of the Spinal Cord. [Updated 2023 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559316/
- Hemmer B, Glocker FX, Schumacher M, et alSubacute combined degeneration: clinical, electrophysiological, and magnetic resonance imaging findingsJournal of Neurology, Neurosurgery & Psychiatry 1998;65:822-827.
- Shah K, Murphy C. Nitrous Oxide Toxicity: Case Files of the Carolinas Medical Center Medical Toxicology Fellowship. J Med Toxicol. 2019 Oct;15(4):299-303. doi: 10.1007/s13181-019-00726-x. Epub 2019 Aug 6. PMID: 31388940; PMCID: PMC6825085.
- Kalmoe MC, Janski AM, Zorumski CF, Nagele P, Palanca BJ, Conway CR. Ketamine and nitrous oxide: The evolution of NMDA receptor antagonists as antidepressant agents. J Neurol Sci. 2020 May 15;412:116778. doi: 10.1016/j.jns.2020.116778. Epub 2020 Mar 19. PMID: 32240970.
- https://www.nytimes.com/2021/01/30/style/nitrous-oxide-whippets-tony-hsieh.html
Read More






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast