Cardionerds: A Cardiology Podcast

364. Case Report: A Drug’s Adverse Effect Unleashes the Wolf – Beth Israel Deaconess Medical Center
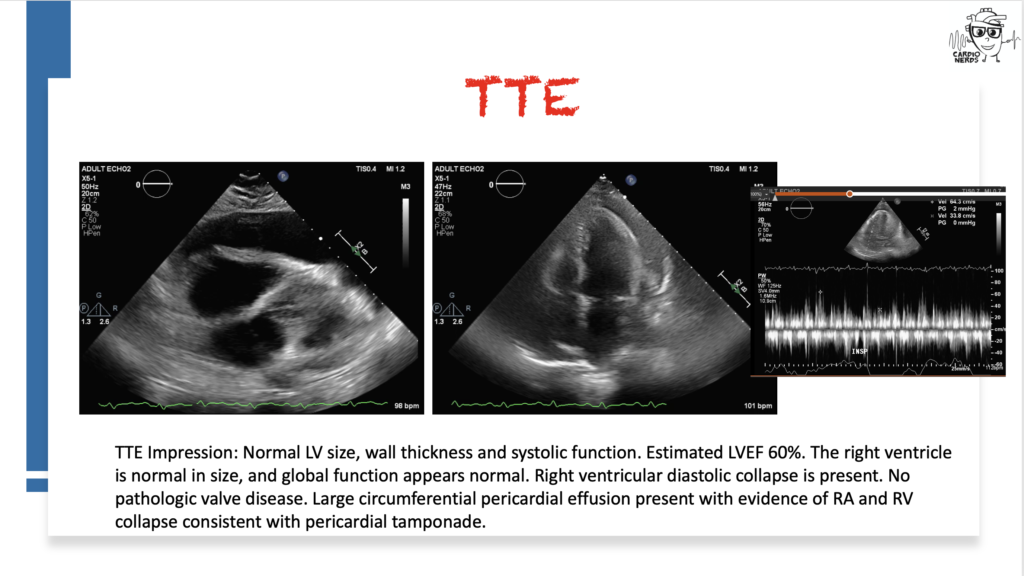
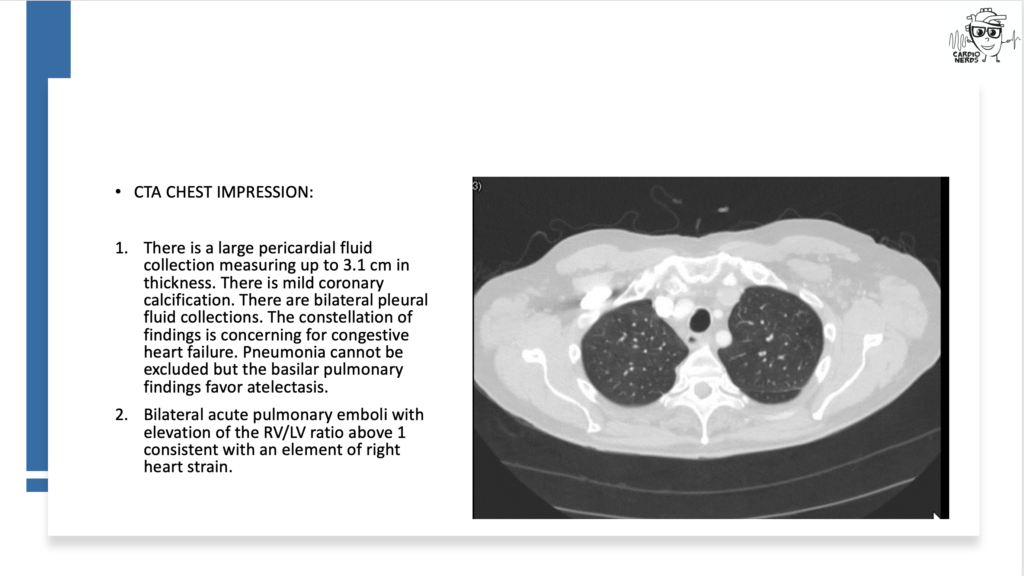
CardioNerds join Dr. Inbar Raber and Dr. Susan Mcilvaine from the Beth Israel Deaconess Medical Center for a Fenway game. They discuss the following case: A 72-year-old man presents with two weeks of progressive dyspnea, orthopnea, nausea, vomiting, diarrhea, and right upper quadrant pain. He has a history of essential thrombocytosis, Barrett’s esophagus, basal cell skin cancer, and hypertension treated with hydralazine. He is found to have bilateral pleural effusions and a pericardial effusion. He undergoes a work-up, including pericardial cytology, which is negative, and blood tests reveal a positive ANA and positive anti-histone antibody. He is diagnosed with drug-induced lupus due to hydralazine and starts treatment with intravenous steroids, resulting in an improvement in his symptoms. Expert commentary is provided by UT Southwestern internal medicine residency program director Dr. Salahuddin (“Dino”) Kazi.
“To study the phenomena of disease without books is to sail an uncharted sea, while to study books without patients is not to go to sea at all.” – Sir William Osler. CardioNerds thank the patients and their loved ones whose stories teach us the Art of Medicine and support our Mission to Democratize Cardiovascular Medicine.
US Cardiology Review is now the official journal of CardioNerds! Submit your manuscript here.
CardioNerds Case Reports Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!
Case Media
Pearls – A Drug’s Adverse Effect Unleashes the Wolf
- The differential diagnosis for pericardial effusion includes metabolic, malignant, medication-induced, traumatic, rheumatologic, and infectious etiologies.
- While pericardial cytology can aid in securing a diagnosis of cancer in patients with malignant pericardial effusions, the sensitivity of the test is limited at around 50%.
- Common symptoms of drug-induced lupus include fever, arthralgias, myalgias, rash, and/or serositis.
- Anti-histone antibodies are typically present in drug-induced lupus, while anti-dsDNA antibodies are typically absent (unlike in systemic lupus erythematosus, SLE).
- Hydralazine-induced lupus has a prevalence of 5-10%, with a higher risk for patients on higher doses or longer durations of drug exposure. Onset is usually months to years after drug initiation.
Show Notes – A Drug’s Adverse Effect Unleashes the Wolf
- There is a broad differential diagnosis for pericardial effusion which includes metabolic, malignant, medication-induced, traumatic, rheumatologic, and infectious etiologies. Metabolic etiologies include renal failure and thyroid disease. Certain malignancies are more likely to cause pericardial effusions, including lung cancer, lymphoma, breast cancer, sarcoma, and melanoma. Radiation therapy to treat chest malignancies can also result in a pericardial effusion. Medications can cause pericardial effusion, including immune checkpoint inhibitors, which can cause myocarditis or pericarditis, and medications associated with drug-induced lupus, such as procainamide, hydralazine, phenytoin, minoxidil, or isoniazid. Trauma can cause pericardial effusions, including blunt chest trauma, cardiac surgery, or cardiac catheterization. Rheumatologic etiologies include lupus, rheumatoid arthritis, systemic sclerosis, sarcoid, and vasculitis. Many different types of infections can cause pericardial effusions, including viruses (e.g., coxsackievirus, echovirus, adenovirus, human immunodeficiency virus, and influenza), bacteria (TB, staphylococcus, streptococcus, and pneumococcus), and fungi. Other must-not-miss etiologies include emergencies like type A aortic dissection and myocardial infarction.
- In a retrospective study of all patients who presented with a hemodynamically significant pericardial effusion and underwent pericardiocentesis, 33% of patients were found to have an underlying malignancy(Ben-Horin et al). Bloody effusion and frank tamponade were significantly more common among patients with malignant effusion, but the overlap was significant, and no epidemiologic or clinical parameter was found useful to differentiate between cancerous and noncancerous effusions. Although this patient’s pericardial fluid cytology was negative, cytology is typically only positive in around 50% of malignant effusions (Ben-Horin et al).
- The risk of drug-induced lupus (DIL) with hydralazine is high, approaching 10% of all treated patients. Another more commonly implicated cardiovascular drug is procainamide, with an incidence of 15-20%. Anti-histone antibodies are typically positive in DIL caused by hydralazine or procainamide, whereas anti-double stranded DNA antibodies are typically absent (in contrast to systemic lupus erythematosus). The most common symptoms of DIL include fever, arthralgias, myalgias, rash, and/or serositis with onset after months to years of drug exposure. If serositis is present, it is more often pleuritis, +/- pericarditis.
- In addition to stopping the offending medication, treatment is extrapolated from the treatment of idiopathic systemic lupus and can include NSAIDs, hydroxychloroquine, and/or systemic steroids, depending on disease severity.
References – A Drug’s Adverse Effect Unleashes the Wolf
- Ben-Horin, Bank, Guetta, & Livneh, A. (2006). Large symptomatic pericardial effusion as the presentation of unrecognized cancer – A study in 173 consecutive patients undergoing pericardiocentesis. Medicine (Baltimore), 85(1), 49–53.
- Borchers, A.T., Keen, C.L. and Gershwin, M.E. (2007), Drug-Induced Lupus. Annals of the New York Academy of Sciences, 1108: 166-182.
- Feng, Glockner, J., et al. (2011). Cardiac Magnetic Resonance Imaging Pericardial Late Gadolinium Enhancement and Elevated Inflammatory Markers Can Predict the Reversibility of Constrictive Pericarditis After Antiinflammatory Medical Therapy A Pilot Study. Circulation (New York, N.Y.), 124(17), 1830–1837






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast