Cardionerds: A Cardiology Podcast

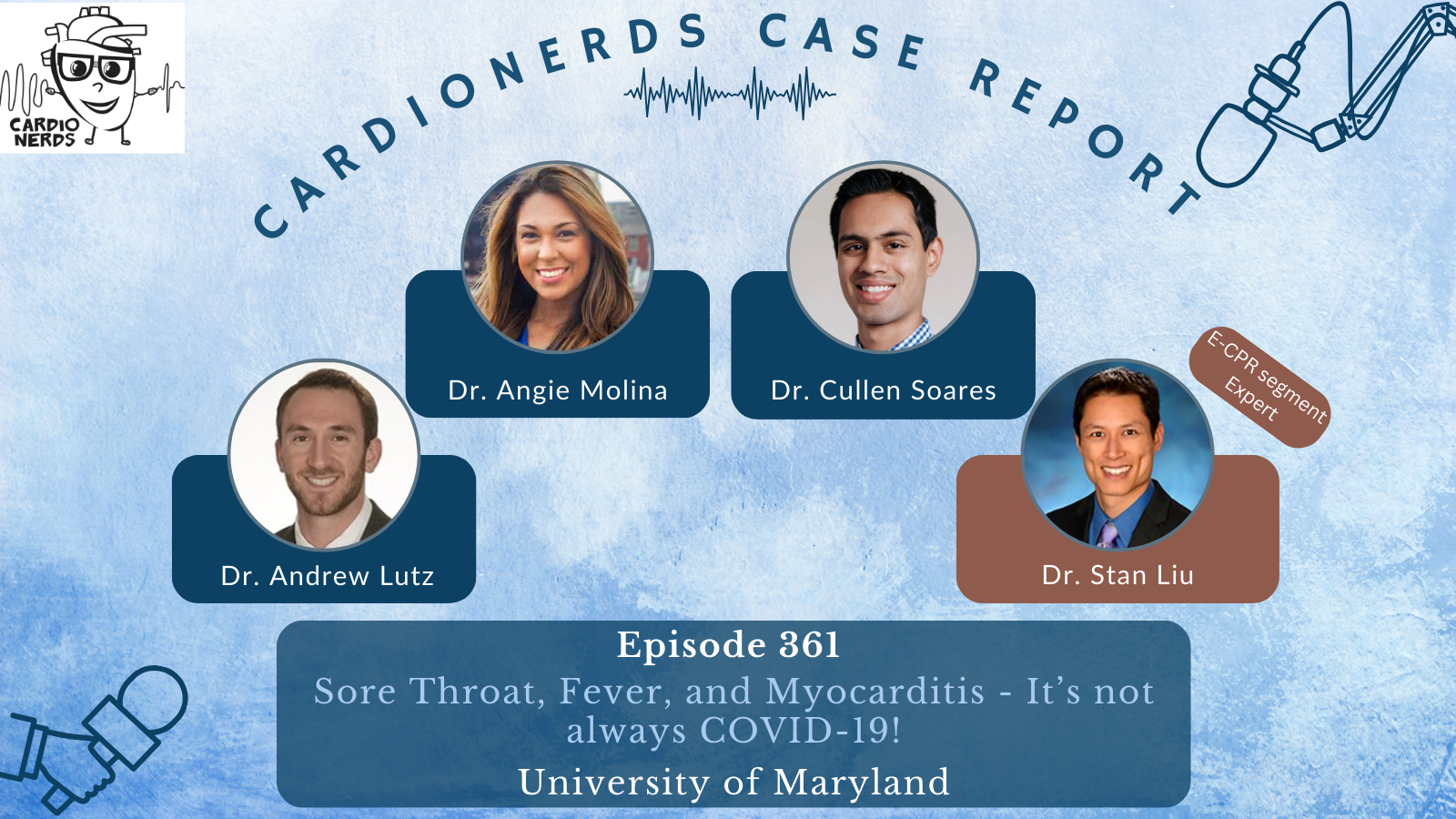
361. Case Report: Sore Throat, Fever, and Myocarditis – It’s not always COVID-19! – University of Maryland
CardioNerds cofounder Dr. Dan Ambinder joins Dr. Angie Molina, Dr. Cullen Soares, and Dr. Andrew Lutz from the University of Maryland Medical Center for some beers and history by Fort McHenry. They discuss a case of disseminated haemophilus influenza
presumed fulminant bacterial myocarditis with mixed septic/cardiogenic shock. Expert commentary is provided by Dr. Stanley Liu (Assistant Professor, Division of Cardiovascular Medicine, University of Maryland School of Medicine). Episode audio was edited by Dr. Chelsea Amo-Tweneboah.
A woman in her twenties with a history of intravenous drug use presented with acute onset fevers and sore throat, subsequently developed respiratory distress and cardiac arrest, and was noted to have epiglottic edema on intubation. She developed shock and multiorgan failure. ECG showed diffuse ST elevations, TTE revealed biventricular dysfunction, and pleural fluid culture grew Haemophilus influenza. Right heart catheterization showed evidence of cardiogenic shock. She improved with supportive care and antibiotics.
“To study the phenomena of disease without books is to sail an uncharted sea, while to study books without patients is not to go to sea at all.” – Sir William Osler. CardioNerds thank the patients and their loved ones whose stories teach us the Art of Medicine and support our Mission to Democratize Cardiovascular Medicine.
US Cardiology Review is now the official journal of CardioNerds! Submit your manuscript here.
CardioNerds Case Reports Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!
Pearls – Sore Throat, Fever, and Myocarditis – It’s not always COVID-19
- The post-cardiac arrest ECG provides helpful information for diagnosing the underlying etiology.
- Be aware of diagnostic biases – availability and anchoring biases are particularly common during respiratory viral (such as COVID-19, RSV) surges.
- Consider a broad differential diagnosis in evaluating myocarditis, including non-viral etiologies.
- Right heart catheterization provides crucial information for diagnosis and management of undifferentiated shock.
- When assessing the need for mechanical circulatory support, consider the current hemodynamics, type of support needed, and risks associated with each type.
Show Notes – Sore Throat, Fever, and Myocarditis – It’s not always COVID-19
- ECG findings consistent with pericarditis include diffuse concave-up ST elevations and downsloping T-P segment (Spodick’s sign) as well as PR depression (lead II), and PR elevation (lead aVR). In contrast, regional ST elevations with “reciprocal” ST depressions and/or Q-waves should raise concern for myocardial ischemia as the etiology.
- Biventricular dysfunction and elevated troponin are commonly seen post-cardiac arrest and may be secondary findings. However, an elevation in troponin that is out of proportion to expected demand ischemia, ECG changes (pericarditis, ischemic ST elevations), and cardiogenic shock suggest a primary cardiac etiology for cardiac arrest.
- The differential diagnosis of infectious myopericarditis includes, most commonly, viral infection (respiratory viruses) and, more rarely, bacterial, fungal, or parasitic. Noninfectious myopericarditis may be autoimmune (such as lupus, sarcoidosis, checkpoint inhibitors), toxin-induced (alcohol, cocaine), and medication-induced (anthracyclines and others).
- Right heart catheterization can help diagnose the etiology of undifferentiated shock, including distinguishing between septic and cardiogenic shock, by providing right and left-sided filling pressures, pulmonary and systemic vascular resistance, and cardiac output.
- Mechanical circulatory support (MCS) is indicated for patients in cardiogenic shock with worsening end-organ perfusion despite inotropic and pressor support. MCS includes intra-aortic balloon pump, percutaneous VAD, TandemHeart, and VA-ECMO. The decision to use specific types of MCS should be individualized to each patient with their comorbidities and hemodynamic profile. Shock teams are vital to guide decision-making.
References
- Witting MD, Hu KM, Westreich AA, Tewelde S, Farzad A, Mattu A. Evaluation of Spodick’s Sign and Other Electrocardiographic Findings as Indicators of STEMI and Pericarditis. J Emerg Med. 2020;58(4):562-569. doi:10.1016/j.jemermed.2020.01.017
- Ferrero P, Piazza I, Lorini LF, Senni M. Epidemiologic and clinical profiles of bacterial myocarditis. Report of two cases and data from a pooled analysis. Indian Heart J. 2020;72(2):82-92. doi:10.1016/j.ihj.2020.04.005
- Pollack A, Kontorovich AR, Fuster V, Dec GW. Viral myocarditis–diagnosis, treatment options, and current controversies. Nat Rev Cardiol. 2015;12(11):670-680. doi:10.1038/nrcardio.2015.108
- Hsu S, Fang JC, Borlaug BA. Hemodynamics for the Heart Failure Clinician: A State-of-the-Art Review. J Card Fail. 2022;28(1):133-148. doi:10.1016/j.cardfail.2021.07.012
- Korabathina R., Heffernan K.S., Paruchuri V., Patel A.R., Mudd J.O., Prutkin J.M., et al: The pulmonary artery pulsatility index identifies severe right ventricular dysfunction in acute inferior myocardial infarction. Catheter Cardiovasc Interv 2012; 80: pp. 593-600. https://pubmed.ncbi.nlm.nih.gov/21954053/
- Drazner MH, Velez-Martinez M, Ayers CR, et al. Relationship of right- to left-sided ventricular filling pressures in advanced heart failure: insights from the ESCAPE trial. Circ Heart Fail. 2013;6(2):264-270. doi:10.1161/CIRCHEARTFAILURE.112.000204






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast