Cardionerds: A Cardiology Podcast

360. Obesity: Lifestyle & Pharmacologic Management of Obesity with Dr. Ambarish Pandey
CardioNerds Dr. Rick Ferraro (CardioNerds Academy House Faculty and Cardiology Fellow at JHH), Dr. Gurleen Kaur (Director of the CardioNerds Internship and Internal Medicine resident at BWH), and Dr. Alli Bigeh (Cardiology Fellow at the Ohio State) as they discuss the growing obesity epidemic and how it relates to cardiovascular disease with Dr. Ambarish Pandey (Cardiologist at UT Southwestern Medical Center). Show notes were drafted by Dr. Alli Bigeh. CardioNerds Academy Intern and student Dr. Shivani Reddy performed audio editing.
Obesity is an important modifiable risk factor for cardiovascular disease, and it is on the rise! Here, we discuss how to identify patients with obesity and develop an approach to address current lifestyle recommendations. We also discuss the spectrum of pharmacologic treatment options available, management strategies, and some therapy options that are on the horizon.
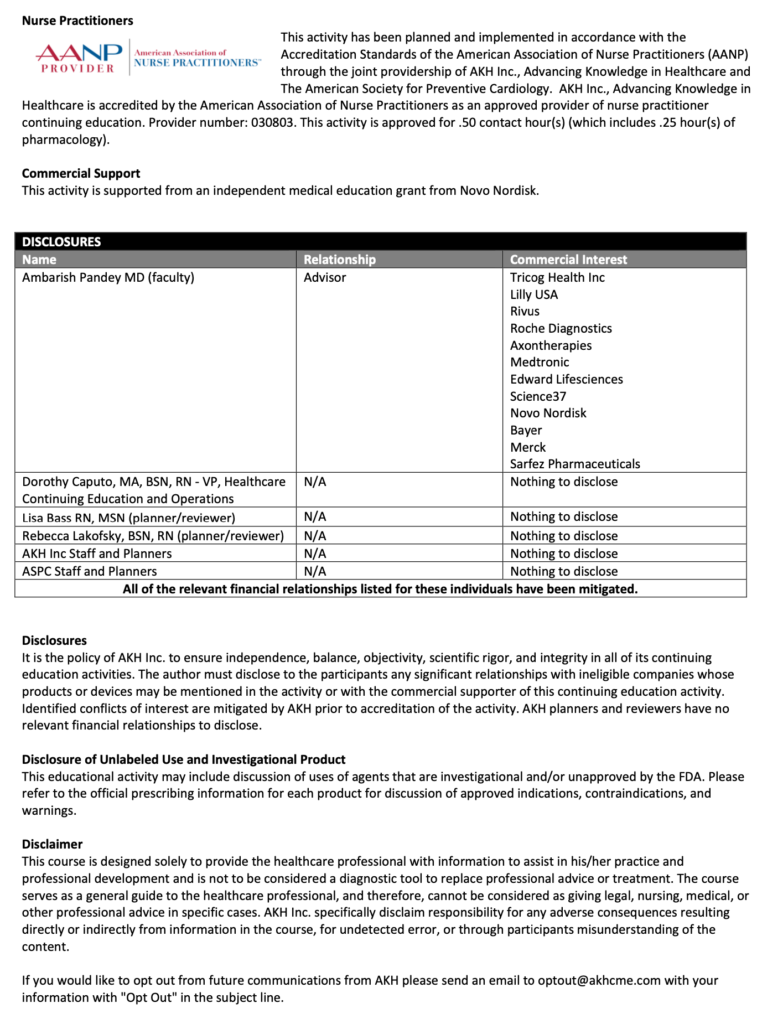
This episode was produced in collaboration with the American Society of Preventive Cardiology (ASPC) with independent medical education grant support from Novo Nordisk. See below for continuing medical education credit.
Claim CME for this episode HERE.
US Cardiology Review is now the official journal of CardioNerds! Submit your manuscript here.
CardioNerds Prevention Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!
Pearls and Quotes – Lifestyle & Pharmacologic Management of Obesity
- Identify obese patients not just using BMI, but also using anthropometric measurements such as waist circumference (central adiposity).
- Lifestyle modifications are our first line of defense against obesity! Current recommendations emphasize caloric restriction of at least 500kcal/day, plant-based and Mediterranean diets, and getting at least 150 minutes of moderate-intensity weekly exercise.
- Dive into the root cause of eating and lifestyle behaviors. It is crucial to address adverse social determinants of health with patients to identify the driving behaviors, particularly among those individuals of low socioeconomic status.
- Newer weight loss agents are most effective at achieving and maintaining substantial weight loss, in particular Semaglutide (GLP-1) and Tirzepatide (GLP-1/GIP). Initiate at a low dose and titrate up slowly.
- Obesity is a risk factor and potential driver for HFpEF. Targeted treatment options for obese patients with HFpEF include SGLT-2 inhibitors and semaglutide, which recently showed improvement in quality of life and exercise capacity in the STEP-HFpEF trial.
Show notes – Lifestyle & Pharmacologic Management of Obesity
How do we identify and define obesity?
- The traditional definition of obesity is based on body mass index (BMI), defined as BMI greater than or equal to 30.0 kg/m2 (weight in kg/height in meters).
- Recognize that BMI may not tell the whole story. A limitation of BMI is it does not reflect differences in body composition and distribution of fat.
- Certain patients may not meet the BMI cutoff for obesity but have elevated cardiovascular risk based on increased central adiposity, specifically those that are categorized as overweight.
- The devil lies in the details of anthropometric parameters. Include waist circumference measurements as part of an obesity assessment of visceral adiposity.
- A waist circumference greater than 40 inches for men and greater than 35 inches for women is considered elevated.
- Recognize that BMI may not tell the whole story. A limitation of BMI is it does not reflect differences in body composition and distribution of fat.
What are some current lifestyle recommendations for obese patients?
- Lifestyle recommendations are the first line of defense against obesity.
- Current ACC/AHA guidelines suggest a target of reducing caloric intake by 500 kcal per day. For patients with severe obesity, this number may be higher.
- Emphasis on hypocaloric plant-based and Mediterranean diets
- Reduce total carbohydrate intake to 50-130 grams per day.
- Focus on a low-fat diet with less than 30% of total energy coming from fat with a high-protein diet to maintain lean mass and promote satiety.
- The overarching theme of prevailing lifestyle recommendations is incorporating whole grains, vegetables, fruit, nuts, and fiber-rich foods while minimizing saturated fats, salt, and sugar intake.
- ACC/AHA recommendations include 150 minutes of moderate-intensity exercise per week.
- Current ACC/AHA guidelines suggest a target of reducing caloric intake by 500 kcal per day. For patients with severe obesity, this number may be higher.
What are some tips for addressing lifestyle modifications with patients?
- Tailor the approach to each individual patient. Get to the root cause and identify barriers to addressing the behaviors.
- Consider getting a psychosocial assessment and focus on behavior modification strategies. Eating behaviors can be associated with other behavioral disorders.
- Patients with severe obesity have a higher risk of adverse cardiovascular events. A risk-based approach for these patients mandates a greater emphasis on weight reduction and caloric restriction.
- Consider access to nutrient-dense food, socioeconomic status, cost of healthy foods, access to exercise resources, and safety of neighborhoods when making recommendations.
- Consider getting a psychosocial assessment and focus on behavior modification strategies. Eating behaviors can be associated with other behavioral disorders.
What are the current pharmacologic options for weight loss? Which are the most effective?
- Consider pharmacological agents once lifestyle modifications and social determinants of health have been addressed. We should not get hung up on lifestyle modifications and fail to progress to using pharmacotherapies or surgical therapies in patients with morbid obesity or cardiovascular disease.
- Pharmacological therapy can be considered in patients with BMI >30 or BMI >27 with comorbidities.
- There are a variety of agents such as Orlistat, Phentermine/Topiramate, Bupropion/Naltrexone, GLP-1 receptor agonists (Liraglutide, Semaglutide) and Tirzepatide (GLP-1/GIP).
- Tirzepatide has the highest amount of reported weight loss, with patients achieving 23% weight loss or up to 50 pounds of weight loss based on the latest SURMOUNT trial. Semaglutide can achieve 16% weight loss based on trial data. The remaining agents have reported weight loss between 6-10%.
- Bariatric surgery should also be considered, especially in patients with severe obesity (BMI >40).
Compare and contrast the GLP-1 agents, specifically semaglutide and liraglutide.
- GLP-1 receptor agonists activate GLP-1 receptors in the pancreas, which increases insulin release, slows gastric emptying, and reduces appetite.
- Semaglutide has a greater weight reduction of up to 16% total weight loss compared to 6% for liraglutide.
- There have been higher reported adverse effects with liraglutide as well. In the STEP-8 trial, the proportion of participants discontinuing treatment for any reason was 13.5% with semaglutide versus 27.6% with liraglutide. Gastrointestinal adverse events were the most common and reported by 84.1% with semaglutide and 82.7% with liraglutide.
- The SELECT trial in patients with preexisting cardiovascular disease and overweight or obesity but without diabetes, weekly subcutaneous semaglutide at a dose of 2.4 mg reduced the incidence of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke by approximately 20%. Liraglutide has been shown to reduce cardiovascular outcomes in patients with established cardiovascular disease but only in patients with diabetes thus far.
- Semaglutide has a greater weight reduction of up to 16% total weight loss compared to 6% for liraglutide.
What other newer agents are on the horizon for treatment of obesity?
- An oral formulation of semaglutide 50mg is currently being tested, with phase 3 results showing up to 15% weight reduction in participants.
- Retatrutide is a new triple-hormone-receptor agonist (an agonist of the glucose-dependent insulinotropic polypeptide [GIP], glucagon-like peptide 1, and glucagon receptors). Phase 2 trial was recently published, reporting up to 25% weight loss in patients.
- Retatrutide is a new triple-hormone-receptor agonist (an agonist of the glucose-dependent insulinotropic polypeptide [GIP], glucagon-like peptide 1, and glucagon receptors). Phase 2 trial was recently published, reporting up to 25% weight loss in patients.
Discuss some strategies to mitigate the GI side effects when using GLP-1 receptor agonists.
- Most importantly- keep a close eye on patient’s symptoms and prepare them for potential side effects along with the mechanism through which they work (i.e., inducing early satiety).
- Expect some degree of gastrointestinal discomfort so patients know what to expect. Side effects often dissipate with continued use of the medication. This can help minimize discontinuation.
- Counsel on diet and nutrition. Patients should eat small food portions for better tolerability, given the effect of the medication to slow gastric emptying.
- Providers should focus on starting at a low dose and titrating up slowly.
- If side effects become intolerable, providers can consider using the last tolerated dose or switching medication classes (i.e. Tirzepatide).
- Expect some degree of gastrointestinal discomfort so patients know what to expect. Side effects often dissipate with continued use of the medication. This can help minimize discontinuation.
References – Lifestyle & Pharmacologic Management of Obesity
- Chakhtoura M, Haber R, Malak G, Caline R, Raya T, Mantzoros CS. Pharmacotherapy of obesity: an update on the available medications and drugs under investigation. Pharmacotherapy of obesity: an update on the available medications and drugs under investigation. 2023;58:101882-101882. doi:https://doi.org/10.1016/j.eclinm.2023.101882
- Després JP, Carpentier AC, Tchernof A, Neeland IJ, Poirier P. Management of Obesity in Cardiovascular Practice. Journal of the American College of Cardiology. 2021;78(5):513-531. doi:https://doi.org/10.1016/j.jacc.2021.05.035
- Dominguez LJ, Veronese N, Di Bella G, et al. Mediterranean diet in the management and prevention of obesity. Experimental Gerontology. 2023;174:112121. doi:https://doi.org/10.1016/j.exger.2023.112121
- Jastreboff AM, Aronne LJ, Ahmad NN, et al. Tirzepatide Once Weekly for the Treatment of Obesity. New England Journal of Medicine. 2022;387(3). doi:https://doi.org/10.1056/nejmoa2206038
- Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults. Circulation. 2013;129(25 suppl 2):S102-S138. doi:https://doi.org/10.1161/01.cir.0000437739.71477.ee
- Kosiborod M, Abildstrøm SZ, Borlaug BA, et al. Semaglutide in Patients with Heart Failure with Preserved Ejection Fraction and Obesity. The New England Journal of Medicine. 2023;389(12). doi:https://doi.org/10.1056/nejmoa2306963
- Lincoff MA, Brown‐Frandsen K, Colhoun HM, et al. Semaglutide and Cardiovascular Outcomes in Obesity without Diabetes. The New England Journal of Medicine. Published online November 11, 2023. doi:https://doi.org/10.1056/nejmoa2307563
- Rubino DM, Greenway FL, Khalid U, et al. Effect of Weekly Subcutaneous Semaglutide vs Daily Liraglutide on Body Weight in Adults With Overweight or Obesity Without Diabetes. JAMA. 2022;327(2):138. doi:https://doi.org/10.1001/jama.2021.23619






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast