Cardionerds: A Cardiology Podcast

355. Case Report: Hypertension With a Twist – Mount Sinai Medical Center
CardioNerds nerd out with Drs. Karishma Rahman (Mount Siani Vascular Medicine fellow), Shu Min Lao (Mount Sinai Rheumatology fellow), and Constantine Troupes (Mount Sinai Vascular Surgery fellow). They discuss the following case: A 20-year-old woman with a history of hypertension (HTN), initially thought to be secondary to a mid-aortic syndrome that resolved after aortic stenting, presents with a re-occurrence of HTN. The case will go through the differential diagnosis of early onset HTN focusing on structural etiologies of HTN, including mid-aortic syndrome and aortitis. We will also discuss the multi-modality imaging used for diagnosis and surveillance, indications and types of procedural intervention, and how to diagnose and treat an underlying inflammatory disorder leading to aortitis. The expert commentary was provided by Dr. Daniella Kadian-Dodov, Associate Professor of Medicine and Vascular Medicine specialist at the Icahn School of Medicine at Mount Sinai. Audo editing was performed by Dr. Chelsea Amo-Tweneboah, CardioNerds Academy Intern and medicine resident at Stony Brook University Hospital.
“To study the phenomena of disease without books is to sail an uncharted sea, while to study books without patients is not to go to sea at all.” – Sir William Osler. CardioNerds thank the patients and their loved ones whose stories teach us the Art of Medicine and support our Mission to Democratize Cardiovascular Medicine.
US Cardiology Review is now the official journal of CardioNerds! Submit your manuscript here.
CardioNerds Case Reports Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!
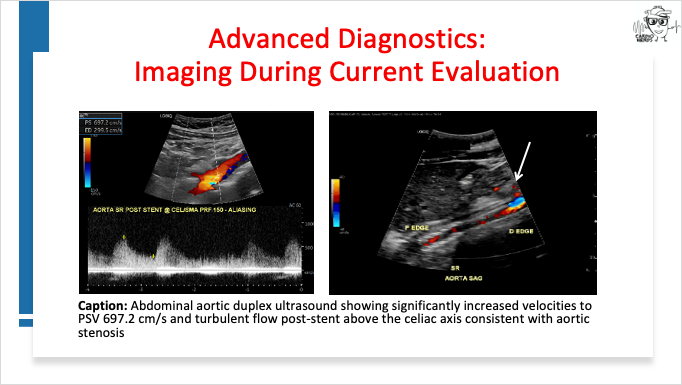
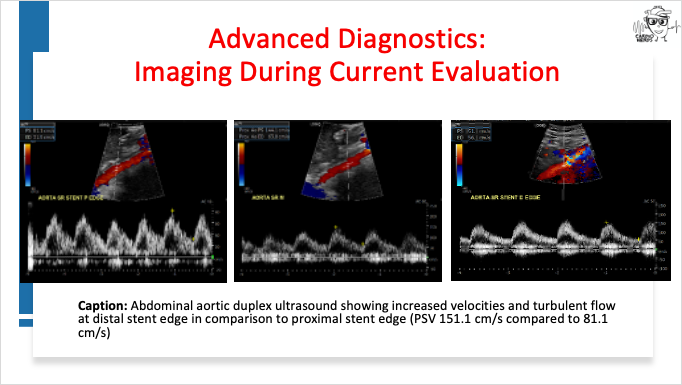
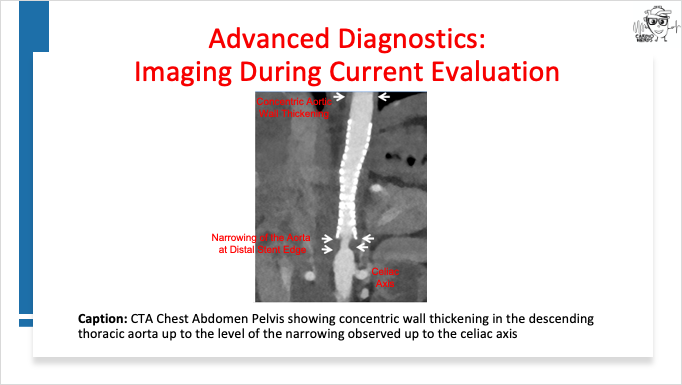
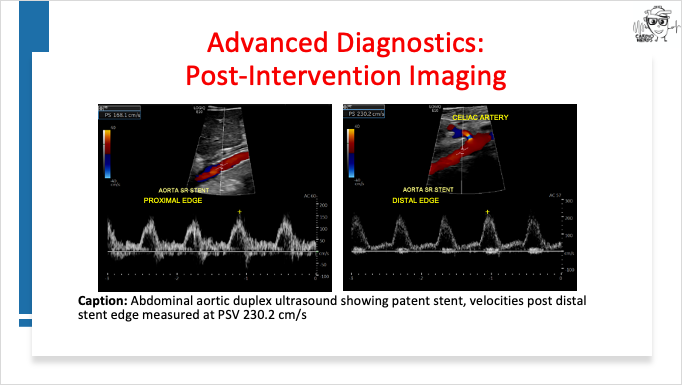
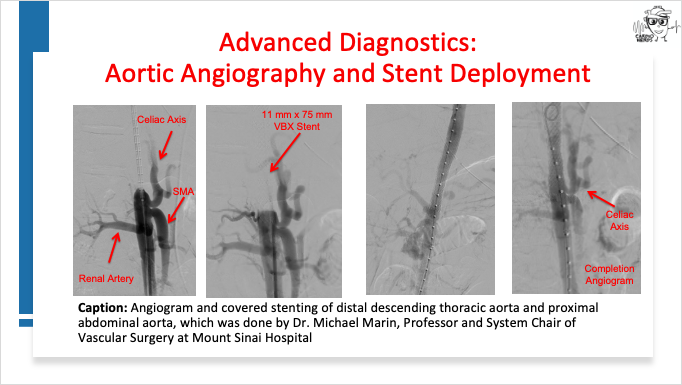
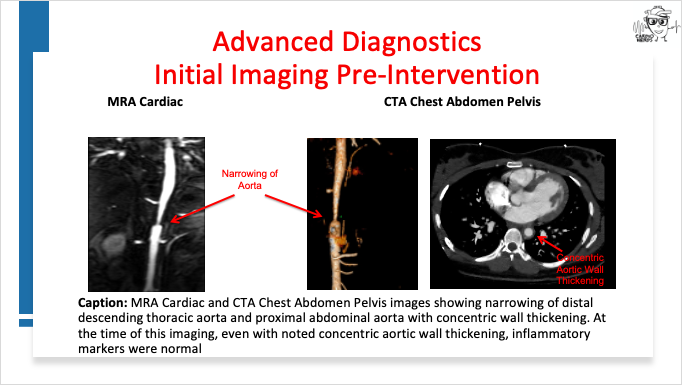
Case Media – Hypertension With a Twist
Pearls – Hypertension With a Twist
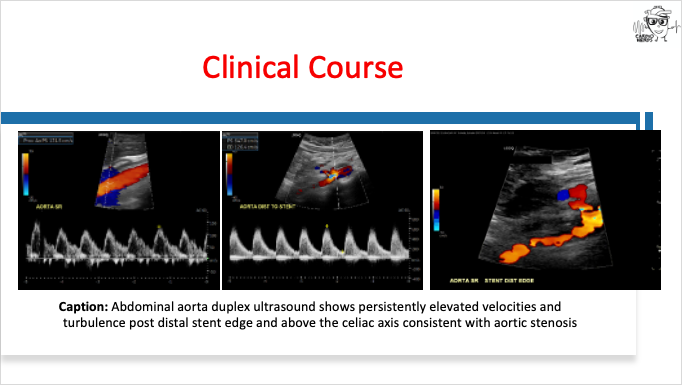
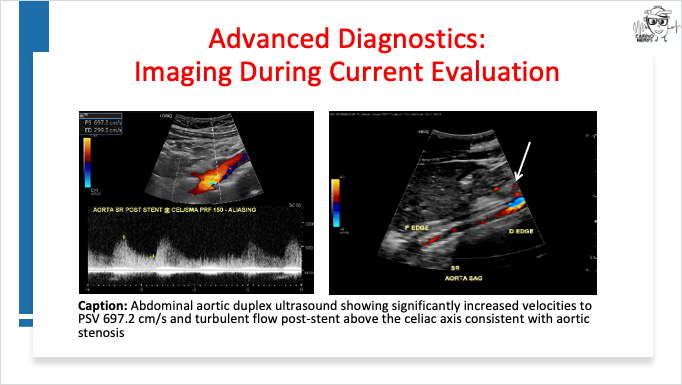
- Early onset hypertension (HTN) and lower extremity claudication should raise suspicion for aortic stenosis (including mid-aortic syndrome). Initial evaluation should include arterial duplex ultrasound and cross-sectional imaging such as CT or MR angiogram of the chest, abdomen, and pelvis to assess for arterial stenosis involving the aorta and/or branching vessels.
- Mid-aortic syndrome can have multiple underlying etiologies. Concentric aortic wall thickening should raise suspicion for an underlying inflammatory disorder. Initial evaluation should include inflammatory markers such as ESR, CRP, and IL-6, but normal values do not exclude underlying aortitis.
- While Takayasu arteritis is the most common inflammatory disorder associated with mid-aortic syndrome, IgG4-RD should also be a part of the differential diagnosis. IgG subclass panel can detect IgG4-RD with elevated serum IgG4 levels, but some cases can require pathology for diagnosis.
- Catheter based intervention is a safe and effective treatment of aortic stenosis for both primary aortic stenosis and post-procedural re-stenosis.
- Multi-modality imaging, including cross-sectional imaging and duplex ultrasound, plays a central role for the diagnosis, management, and post-procedural surveillance of aortic disease.
- A multi-disciplinary team (as exemplified by the participants of this podcast!) is essential for the management of complex aortopathy cases to optimize clinical outcomes.
Show Notes – Hypertension With a Twist
1. Early onset HTN can have multiple etiologies – aortic stenosis (including but not limited to secondary to congenital aortic coarctation and mid–aortic syndrome, as well as in stent re-stenosis if there is a history of aortic stenting), thrombosis, infection, inflammatory/autoimmune disorders, renovascular disease, polycystic kidney disease, and endocrine disorders.
2. Mid-aortic syndrome is characterized by segmental or diffuse narrowing of the abdominal and/or distal descending aorta with involvement of the branches of the proximal abdominal aorta (renal artery, celiac artery, superior mesenteric artery) and represents approximately 0.5 to 2% of all cases of aortic narrowing. Underlying etiologies include genetic syndromes, inflammatory, non-inflammatory, and idiopathic. It is important to have a high suspicion of underlying inflammatory disorders if cross-sectional imaging reveals concentric aortic wall thickening1,2.
3. The current treatment options for aortic stenosis (of the aorta here…not the aortic valve) include balloon angioplasty, aortic stenting, and surgical repair. While studies show the efficacy of balloon angioplasty and aortic stenting, data is limited as studies were mostly done in children3,4.
4. Aortitis5-16 can have multiple etiologies including infectious (such as TB, syphilis, HIV, bacterial, fungal), inflammatory disorders (such as large vessel vasculitis, IgG4-RD, Behcet syndrome, relapsing polychondritis, spondyloarthritis, SLE, and rheumatoid arthritis), and idiopathic. Sometimes, hereditary connective tissue disorders (such Marfan syndrome,, Ehlers-Danlos syndrome, and Loeys-Dietz syndrome) are included in the differential diagnosis, however, they would present as an aortic intramural hematoma (IMH) that typically would appears as eccentric wall thickening (rather than concentric wall thickening more consistent with aortitis).
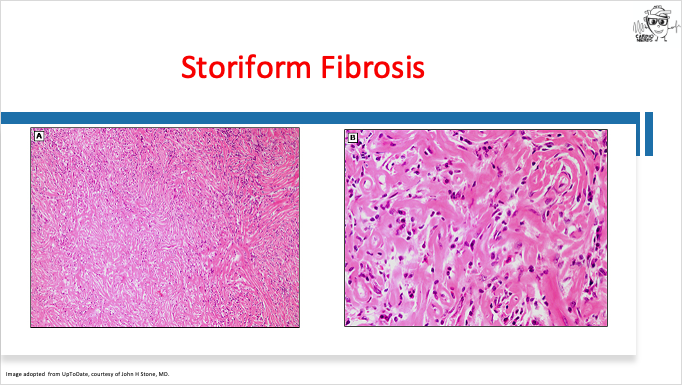
5. While Takayasu arteritis is the most common inflammatory disorder associated with mid-aortic syndrome, IgG4-RD should also be a part of the differential diagnosis. IgG4-RD is characterized by lymphoplasmacytic infiltrates featuring IgG4 positive plasma cells. It presents in predominantly males between ages 40-70 years of age. The rate of vascular involvement is approximately 8% for aortitis and 20-36% periaortitis. It can be diagnosed with elevated serum IgG4 levels or from tissue biopsy where pathology would show dense lymphoplasmacytic infiltrates in a storiform fibrosis pattern with obliterative phlebitis and >40% plasma calls and >10 positive plasma cells/high power field. It is treated initially treated with high dose steroids with transition to steroid sparing agents such as Rituximab (RTX), azathioprine, mycophenolate, and methotrexate with RTX being the preferred agent10,14.
6. In cases of re-stenosis after initial balloon angioplasty and stenting, indications for re-intervention include hypertension in the setting of imaging evidence of re-stenosis (e.g. > 50% percent aortic narrowing relative to the aortic diameter at the diaphragm level) and
pressure gradient across the coarctation > 20 mmHg. The timing of re-intervention in cases of aortitis secondary to underlying inflammatory disorders will require a multi-disciplinary discussion to determine when underlying inflammatory disorder is sufficiently controlled for re-intervention.
References – Hypertension With a Twist
- Bacha E, Hijazi ZM. Management of Coarctation of the Aorta. U: UpToDate, Fulton DR ed UpToDate [Internet] Waltham, MA: UpToDate. 2020.
- Lazea C, Al-Khzouz C, Sufana C, et al. Diagnosis and management of genetic causes of middle aortic syndrome in children: a comprehensive literature review. Therapeutics and Clinical Risk Management. 2022:233-248.
- Rodés-Cabau J, Miró J, Dancea A, et al. Comparison of surgical and transcatheter treatment for native coarctation of the aorta in patients≥ 1 year old. The Quebec Native Coarctation of the Aorta Study. American heart journal. 2007;154(1):186-192.
- Meadows J, Minahan M, McElhinney DB, McEnaney K, Ringel R. Intermediate outcomes in the prospective, multicenter Coarctation of the Aorta Stent Trial (COAST). Circulation. 2015;131(19):1656-1664.
- Nikiphorou E, Galloway J, Fragoulis GE. Overview of IgG4-related aortitis and periaortitis. A decade since their first description. Autoimmunity reviews. 2020;19(12):102694.
- Kadian-Dodov D, Seo P, Robson PM, Fayad ZA, Olin JW. Inflammatory Diseases of the Aorta: JACC Focus Seminar, Part 2. Journal of the American College of Cardiology. 2022;80(8):832-844.
- Sohrabi B, Jamshidi P, Yaghoubi A, et al. Comparison between covered and bare Cheatham-Platinum stents for endovascular treatment of patients with native post-ductal aortic coarctation: immediate and intermediate-term results. JACC: Cardiovascular Interventions. 2014;7(4):416-423.
- Marvisi C, Buttini EA, Vaglio A. Aortitis and periaortitis: the puzzling spectrum of inflammatory aortic diseases. La Presse Médicale. 2020;49(1):104018.
- Bossone E, Pluchinotta FR, Andreas M, et al. Aortitis. Vascular pharmacology. 2016;80:1-10.
- Carruthers MN, Topazian MD, Khosroshahi A, et al. Rituximab for IgG4-related disease: a prospective, open-label trial. Annals of the rheumatic diseases. 2015;74(6):1171-1177.
- Wallace ZS, Perugino C, Matza M, Deshpande V, Sharma A, Stone JH. Immunoglobulin G4–related disease. Clinics in chest medicine. 2019;40(3):583-597.
- Wallace ZS, Naden RP, Chari S, et al. The 2019 American College of Rheumatology/European league against rheumatism classification criteria for IgG4‐related disease. Arthritis & Rheumatology. 2020;72(1):7-19.
- Onen F, Akkoc N. Epidemiology of Takayasu arteritis. La Presse Médicale. 2017;46(7-8):e197-e203.
- Ebbo M, Grados A, Samson M, et al. Long-term efficacy and safety of rituximab in IgG4-related disease: data from a French nationwide study of thirty-three patients. PLoS One. 2017;12(9):e0183844.
- Maz M, Chung SA, Abril A, et al. 2021 American College of Rheumatology/Vasculitis Foundation guideline for the management of giant cell arteritis and Takayasu arteritis. Arthritis Care & Research. 2021;73(8):1071-1087.
- Lupi-Herrera E, Sanchez-Torres G, Marcushamer J, Mispireta J, Horwitz S, Vela JE. Takayasu’s arteritis. Clinical study of 107 cases. American heart journal. 1977;93(1):94-103.






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast