Cardionerds: A Cardiology Podcast

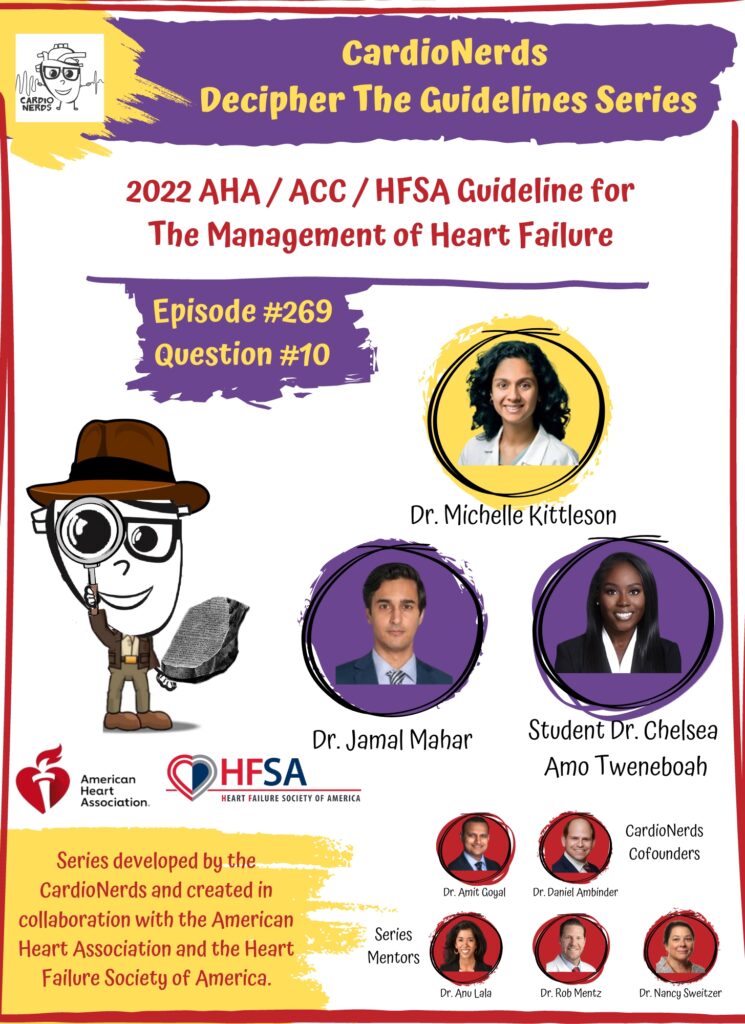
269. Guidelines: 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure – Question #10 with Dr. Michelle Kittleson
The following question refers to Section 7.7 of the 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure.
The question is asked by St. George’s University medical student and CardioNerds Intern Chelsea Tweneboah, answered first by Baylor College of Medicine Cardiology Fellow and CardioNerds Ambassador Dr. Jamal Mahar, and then by expert faculty Dr. Michelle Kittleson.
Dr. Kittleson is Director of Education in Heart Failure and Transplantation, Director of Heart Failure Research, and Professor of Medicine at the Smidt Heart Institute, Cedars-Sinai. She is Deputy Editor of the Journal of Heart and Lung Transplantation, on Guideline Writing Committees for the American College of Cardiology (ACC)/American Heart Association, is the Co Editor-in-Chief for the ACC Heart Failure Self-Assessment Program, and on the Board of Directors for the Heart Failure Society of America. Her Clinician’s Guide to the 2022 Heart Failure guidelines, published in the Journal of Cardiac Failure, are a must-read for everyone!
The Decipher the Guidelines: 2022 AHA / ACC / HFSA Guideline for The Management of Heart Failure series was developed by the CardioNerds and created in collaboration with the American Heart Association and the Heart Failure Society of America. It was created by 30 trainees spanning college through advanced fellowship under the leadership of CardioNerds Cofounders Dr. Amit Goyal and Dr. Dan Ambinder, with mentorship from Dr. Anu Lala, Dr. Robert Mentz, and Dr. Nancy Sweitzer. We thank Dr. Judy Bezanson and Dr. Elliott Antman for tremendous guidance.
Ms. Heffpefner is a 54-year-old woman who comes to your office for a routine visit. She does report increased fatigue and dyspnea on exertion without new orthopnea or extremity edema. She was previously diagnosed with type 2 diabetes, morbid obesity, obstructive sleep apnea, and TIA. She is currently prescribed metformin 1000mg twice daily, aspirin 81mg daily, rosuvastatin 40mg nightly, and furosemide 40mg daily. In clinic, her BP is 140/85 mmHg, HR is 110/min (rhythm irregularly irregular, found to be atrial fibrillation on ECG), and BMI is 43 kg/m2. Transthoracic echo shows an LVEF of 60%, moderate LV hypertrophy, moderate LA enlargement, and grade 2 diastolic dysfunction with no significant valvulopathy. What is the best next step?
A
Provide reassurance
B
Refer for gastric bypass
C
Refer for atrial fibrillation ablation
D
Start metoprolol and apixaban
Explanation
The correct answer is D – start metoprolol and apixaban.
Ms. Hefpeffner has a new diagnosis of atrial fibrillation (AF) and has a significantly elevated risk for embolic stroke based on her CHA2DS2-VASc score of 6 (hypertension, diabetes, heart failure, prior TIA, and female sex). The relationship between AF and HF is complex and the presence of either worsens the status of the other. Managing AF in patients with HFpEF can lead to symptom improvement (Class 2a, LOR C-EO). However, large, randomized trial data are unavailable to specifically guide therapy in patients with AF and HFpEF.
Generally, management of AF involves stroke prevention, rate and/or rhythm control, and lifestyle / risk-factor modification. With regards to stroke prevention, patients with chronic HF with permanent-persistent-paroxysmal AF and a CHA2DS2-VASc score of ≥2 (for men) and ≥3 (for women) should receive chronic anticoagulant therapy (Class 1, LOE A). When anticoagulation is used in chronic HF patients with AF, a DOAC is recommended over warfarin in eligible patients (Class 1, LOE A).
The decision for rate versus rhythm control should be individualized and reflects both patient symptoms and the likelihood of better ventricular function with sinus rhythm. For patients with HF and symptoms caused by AF, AF ablation is reasonable to improve symptoms and QOL (Class 2a, LOE B-R). However, referring for catheter ablation would be premature before first attempting rate control and instituting anticoagulation therapy.
Traditionally, beta-blockers and nondihydropyridine calcium channel blockers are used as first-line agents for rate control in AF. Interestingly, a small open-label trial, RATE-AF in elderly patients with AF and symptoms of HF (mostly with preserved LVEF), compared bisoprolol to digoxin. Although the primary endpoint of quality of life at 6 months was similar between the 2 groups, several secondary QOL endpoints, functional capacity, and reduction in NT-proBNP favored digoxin at 12 months, with similar rate reductions in both groups. More side effects (such as dizziness, lethargy, and hypotension) were seen with bisoprolol than with digoxin. However, digoxin has a narrow therapeutic window and needs to be monitored more closely.
Option A (provide reassurance) is inappropriate as this patient has heart failure with preserved EF, defined by signs and symptoms of HF in patients with an LVEF of 50% or more. Echocardiogram hints in this case include LV hypertrophy and diastolic dysfunction. Our patient also has comorbidities frequently associated with HFpEF such as hypertension, diabetes, OSA, and obesity. Other common comorbidities include CAD, CKD, and atrial arrhythmias. When diagnosing HFpEF, care must be taken to rule out mimicking conditions such as pulmonary hypertension or amyloidosis. A large portion of the management of HFpEF includes managing comorbid conditions such as hypertension, OSA, and atrial fibrillation. At this time, she is symptomatic with atrial fibrillation and rapid ventricular response, and warrants both rate control and stroke prophylaxis.
Although gastric bypass should be considered for patients with a BMI >35 kg/m2 with comorbidities (such as HTN or diabetes) and patients with a BMI > 40 kg/m2 independent of comorbid conditions, this is not the best next step at this time. First, she should receive anticoagulation to reduce the risk of stroke and achieve better control of her HR and BP.
Patients with HFpEF and hypertension should have medication titrated to attain blood pressure targets in accordance with published clinical practice guidelines to prevent morbidity (Class 1, LOE C-LD). Although the optimal BP goal and antihypertensive regimen in patient with HFpEF is not known, HFpEF trials so far have shown that RAAS antagonists including ACEi, ARB, MRA and possibly ARNi could be first-line agents to treat HTN in patients with HFpEF. Beta blockers may be used to treat hypertension in patients with a history of
MI, symptomatic CAD, or AF with rapid ventricular response. These effects need to be balanced with the potential contribution of chronotropic incompetence to exercise intolerance in some patients.
Main Takeaway
In patients with HFpEF, the diagnosis and management of comorbidities are very important, especially the treatment of HTN (Class 1, LOE C-LD) and AF (Class 2a, LOE C-EO).
Guideline Loc.
Section 7.7.1, Figure 12
Section 10.2
Decipher the Guidelines: 2022 Heart Failure Guidelines Page
CardioNerds Episode Page
CardioNerds Academy
Cardionerds Healy Honor Roll
CardioNerds Journal Club
Subscribe to The Heartbeat Newsletter!
Check out CardioNerds SWAG!
Become a CardioNerds Patron!






 Visit Podcast Website
Visit Podcast Website RSS Podcast Feed
RSS Podcast Feed Subscribe
Subscribe
 Add to MyCast
Add to MyCast